Eccrine Poroma in the Breast Mimicking Malignancy: A Case Report and Review of the Literature
Amal Benchine1, Najwa Loukili1, Samia Sassi2, El Hassouni Fatima1, Mouniya El Youssfi1 and Samir Bargach1
1Department of Obstetrics and Gynecology, Mohammed V University, Rabat, Morocco 2Department of Pathology, Mohammed V University, Rabat, Morocco
DOIDOI: 10.36648/2471-9803.10.1.13
Amal Benchine1*, Najwa Loukili1, Samia Sassi2, El Hassouni Fatima1, Mouniya El Youssfi1 and Samir Bargach1
1Department of Obstetrics and Gynecology, Mohammed V University, Rabat, Morocco
2Department of Pathology, Mohammed V University, Rabat, Morocco
- *Corresponding Author:
- Amal Benchine
Department of Obstetrics and Gynecology, Mohammed V University, Rabat,
Morocco,
E-mail: drbenchineamal@gmail.com
Received date: July 18, 2024, Manuscript No. IPCCO-24-19423; Editor assigned date: July 22, 2024, PreQC No. IPCCO-24-19423 (PQ); Reviewed date: August 05, 2024, QC No. IPCCO-24-19423; Revised date: August 12, 2024, Manuscript No. IPCCO-24-19423 (R); Published date: August 19, 2024, DOI: 10.36648/2471-9803.10.1.133
Citation: Amal B, Najwa L, Samia T, Samia S, Hassouni FE, et al. (2024) Eccrine Poroma in the Breast Mimicking Malignancy: A Case Report and Review of the Literature. Crit Care Obst Gyne Vol.10 No.1: 133.
Abstract
Introduction: Eccrine Poroma (EP) is a rare benign adnexal neoplasm originating from the intra-epidermal portion of the sweat gland duct. The breast is an extremely rare site for this tumor, with only one reported case in the literature. This report highlights its unusual clinical presentation, surgical approach and follow-up.
Objective: Aim of this study is to present a case report of EP involving the breast and to review the existing literature on this rare cutaneous neoplasm in atypical anatomical locations.
Materials and methods: A 66-year-old woman presented with a slow-growing cutaneous lesion on her left breast. Clinical examination revealed a pink bluish dome-shaped nodule. Imaging studies was suggestive of breast tumor with low suspicion of malignancy. Histopathological examination and immunohistochemical staining confirm the diagnostic of eccrine poroma. Surgical excision with clear margins was performed and no recurrence or malignant transformation was observed.
Results: Eccrine poroma of the breast is a rare benign tumor that can present diagnostic challenges, particularly when they mimic malignant lesions clinically and radiologically. Histopathological examination remains the gold standard for diagnosis, immunohistochemical staining can further support the diagnosis. Treatment typically involves surgical excision with clear margins and prognosis is excellent, with low rates of recurrence or malignant transformation.
Conclusion: EP is known as the great imitator due to its clinical and dermoscopic diversity. Despite its rare occurrence, EP should be considered in the differential diagnosis of a slowly growing breast mass with typical clinical features.
Keywords
Eccrine poroma; Breast; Sweat gland neoplasms; Surgical excision; Porocarcinoma; Case report
Introduction
Eccrine poroma is a benign adnexal neoplasm originating from the intra-epidermal portion of the eccrine gland duct, known as the acrosyringium [1]. It is typically slow growing and tends to occur in the middle-aged and elderly individuals, with no sex predilection [1,2]. Eccrine poroma may arise in any skin area containing sweat glands, but it is most commonly found on acral sites such as the soles and palms [3]. Despite its rarity, the natural history of eccrine poroma is understudied, however this tumor with a benign appearance can progress to its malignant counterpart; porocarcinoma [3,4].
To the best of our knowledge’s, breast is an extremely rare site for EP, with only one reported case in the literature [5]. Here, we present a case of eccrine poroma arising in the breast, initially misdiagnosed as breast cancer. We highlight its clinical features, surgical management and follow-up processes.
Our work has been reported in line with the SCARE Guidelines 2023 criteria [6].
Case Report
A 66-years-old woman was admitted to our university hospital’s gynecology ward with a 3 years history of an asymptomatic slow growing cutaneous lesion on the left breast.
The patient has a 6 years history of systemic arterial hypertension on drug therapy. She also underwent a thyroidectomy and has been under treatment for 30 years. She did not have a family history of breast carcinoma, trauma or surgery.
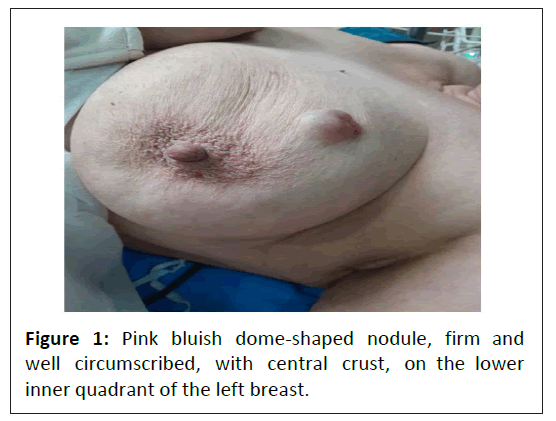
Physical examination revealed on the upper inner quadrant of the left breast a pink bluish dome-shaped nodule, firm and well circumscribed, with central crust, measuring approximately 1 cm × 1 cm (Figure 1). There were no palpable lump or skin lesion on the nipple and areola. The right breast was normal and axillary lymphadenopathy was absent.
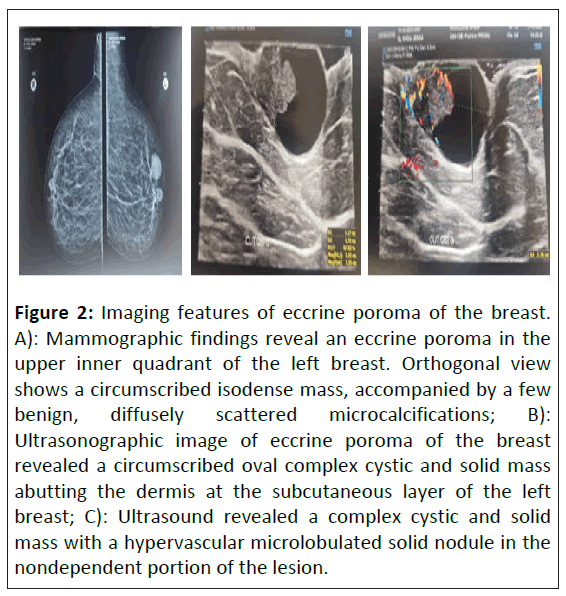
Subsequent mammogram images showed on the left breast a circumscribed isodense mass, associated with few benign, diffusely scattered micro calcifications. Ultrasonography revealed a 1.5 cm × 2 cm circumscribed oval complex cystic and solid mass abutting the dermis at the subcutaneous layer of the left breast, featuring a hyper vascular mural nodule situated in the non-dependent portion of the lesion. Radiologically, it was considered Breast Imaging Reporting and Data System (BI-RADS) Category 4A (low suspicion of malignancy) (Figure 2).
Figure 2: Imaging features of eccrine poroma of the breast. A): Mammographic findings reveal an eccrine poroma in the upper inner quadrant of the left breast. Orthogonal view shows a circumscribed isodense mass, accompanied by a few benign, diffusely scattered microcalcifications; B): Ultrasonographic image of eccrine poroma of the breast revealed a circumscribed oval complex cystic and solid mass abutting the dermis at the subcutaneous layer of the left breast; C): Ultrasound revealed a complex cystic and solid mass with a hypervascular microlobulated solid nodule in the nondependent portion of the lesion.
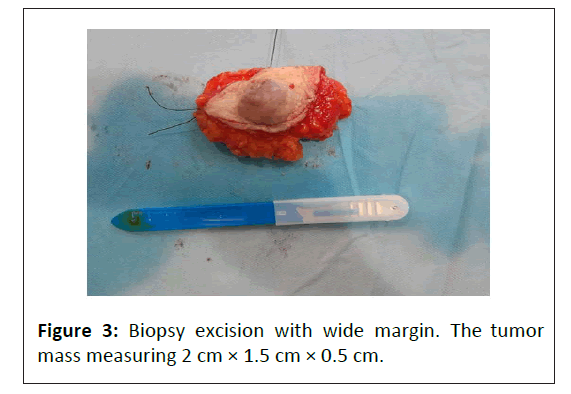
Surgical excision was performed under general anaesthesia and was wide, ensuring a sufficient margin of healthy tissue around the lesion (Figure 3).
Macroscopically, the lesion appeared as a well-circumscribed non-encapsulated brownish mass, consisted of a combination of solid and cystic areas, measuring 2.8 cm × 1.9 cm × 0.6 cm.
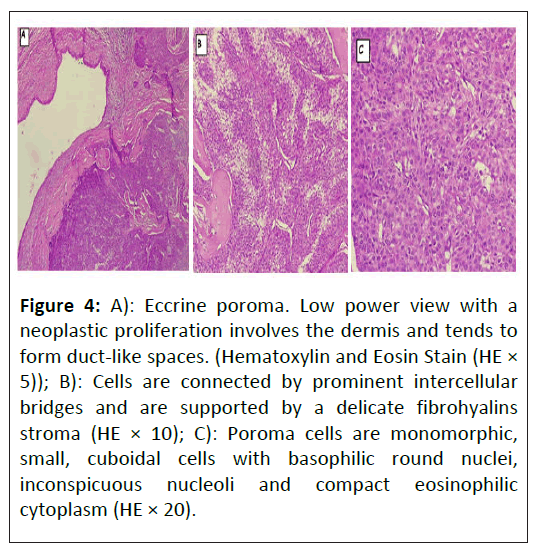
Histopathologic examination of the specimen revealed a dermal tumor consisting of small basaloid epithelial cells. These cells displayed uniform ovoid nuclei with fine chromatin and few visible mitotic figures. The tumor extended from the epidermis to a cystic ductal structure with regular epithelial borders, situated within a highly vascularized stroma. The surgical margins were tumour-free (Figure 4).
Figure 4: A): Eccrine poroma. Low power view with a neoplastic proliferation involves the dermis and tends to form duct-like spaces. (Hematoxylin and Eosin Stain (HE × 5)); B): Cells are connected by prominent intercellular bridges and are supported by a delicate fibrohyalins stroma (HE × 10); C): Poroma cells are monomorphic, small, cuboidal cells with basophilic round nuclei, inconspicuous nucleoli and compact eosinophilic cytoplasm (HE × 20).
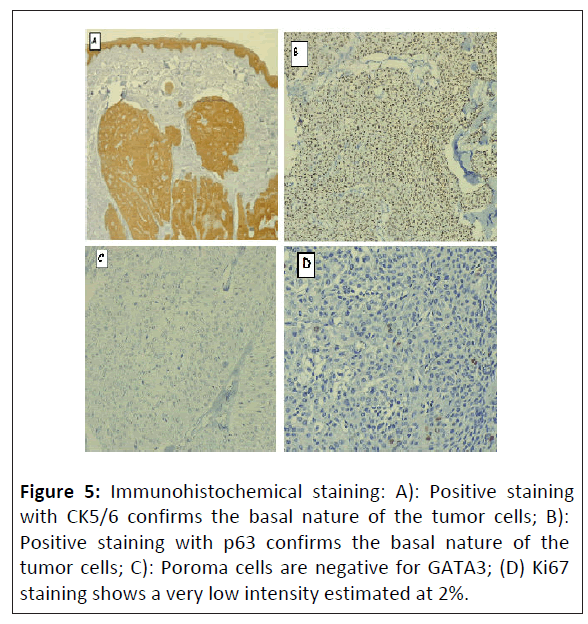
Immunohistochemical staining was negative for GATA-3 and RE, focally positive for Ki67 and diffusely positive for p63, CK5/6, CK14 and EMA Ab-3 (Figure 5).
The diagnosis of eccrine poroma with no evidence of malignancy was made. No recurrence or malignant transformation occurred within 6-month follow-up.
Results and Discussion
Eccrine poroma, initially described by Goldman, et al. is a rare benign cutaneous tumor arising from the acrosyringium, the intraepidermal segment of the eccrine sweat duct. It represents approximately 10% of sweat gland tumors and less than 1% of all skin diseases, with no ethnic or sex predilection [1,7]. Although EP is typically found on acral sites, the lesion has been sporadically reported in other areas such as the head, scalp, eyelids, nose, neck, upper limbs and trunk, including one report in the inframmary area of the chest [5,7]. The breast is an extremely rare primary site for the disease.
The exact etiology of EP remains unclear, but it is believed to potentially be linked to multiple factors such as radiation exposure, trauma, pregnancy, certain chemotherapy medications and infection with human papillomavirus [1]. It has also been sporadically associated with additional conditions, including Bowen’s disease and hypohidrotic ectodermal dysplasia, contrarily, there is no identified familial predisposition for poroma development [4]. Our patient had no previously described risk factors.
Clinically, it usually appears as an asymptomatic mild solitary slow-growing papule, nodule or plaque with colors ranging from skin color to red to brown or bluish [4]. It is typically slow growing with the protruding lesion ranging in diameter from a few millimeters to 2 centimeters and its surface is usually smooth or slightly lobulated [1].
Clinical diagnosis of EPs can be difficult, especially when they occur in non-volar areas. In such cases, EP may be misdiagnosed as malignant melanoma, Basal Cell Carcinoma (BCC), or Squamous Cell Carcinoma (SCC). Dermoscopy can help diagnose poroma, although specific dermoscopic features of EP have not yet been fully elucidated [8]. The main dermoscopic feature of non-pigmented poromas is the vascular pattern, which includes various structures like polymorphic, glomerular, leaf- and flowerlike, linear-irregular and looped or hairpin like formations. Poromas typically show less distinct vascular structures compared to basal cell carcinoma, indicating a deeper dermal location and assisting in differential diagnosis [9].
Histologically, EP appears as a well-defined tumor with proliferating cuboidal or poroid cells, often extending from the basal epidermis into the dermal layer. There are four variants based on the location of poroid cells relative to the epidermis: Eccrine poroma, poroid hidradenoma, hidroacanthoma simplex and dermal duct tumor [10].
Poroid cells are cuboidal keratinocytes, exhibiting a pattern characterized by non-palisading and uniform ovoid nuclei with discrete nucleoli. Typically, the cytoplasm is eosinophilic and shows positive staining with Periodic Acid Schiff (PAS). Carcinoembryonic antigen immunostaining is used to confirm the presence of ductal differentiation in poromas, which varies greatly among these tumors [11].
Although EP is usually benign, it has a potential progression into a malignant form known as eccrine porocarcinoma, exhibiting recent changes such as ulceration, bleeding, sudden growth [3,12]. It is considered a rare and extremely invasive cutaneous tumour that represent 0.005% to 0.01% of all skin cancers [13]. Eccrine Porocarcinoma (EPC) typically arises from a pre-existing poroma, however it can also develop de novo [12]. It often presents as rapidly growing, ulcerating polypoid, protruding growths or verrucous plaques, commonly located on the limbs and scalp [12,13]. Due to its multiple clinical and histopathological mimics, EPC can be misdiagnosed as SCC, Bowen's disease, seborrheic keratosis, or pyogenic granuloma particularly when it presents in uncommon locations such as the breast [13,14].
EPC is characterized by its highly invasive and metastatic potential, with the lymph nodes (57.7%) and lungs (12.8%) being the most common sites for metastasis [15].
Treatment of poroma is optional but typically curative, since it is a benign skin growth [11]. There are several nonsurgical methods for this tumor, including laser therapy, electrocautery and cryotherapy using liquid nitrogen [1]. But surgical excision remains the optimal treatment option [11]. Recurrence of eccrine poroma is rare, unlike its malignant counterpart [5]. On the contrary, the primary treatment for eccrine porocarcinoma is wide surgical excision with broad tumor margins, which achieves therapeutic outcomes in 70%-80% of cases [15]. However, there is currently no evidence-based consensus on recommended excision margins, although it is generally believed that surgical margins that reduce the recurrence rate range from 3 to 10 mm [9]. There are other treatment modalities for porocarcinoma, including Mohs micrographic surgery electrocautery, electrofulguration, radiation and amputation [5].
Recurrence of eccrine poroma is rare compared to its malignant counterpart, which has a local recurrence estimated to occur in 20% to 35% of cases, with lymph node metastasis observed in 20% and solid organ metastasis in 10%. The high rate of lymph node metastasis may support regional lymph node dissection, but there are still insufficient data to recommend this procedure as routine.
Adjuvant therapies including chemotherapy and radiotherapy have been reserved for metastatic disease and recurrence [15].
It’s important to highlight the necessity of regular follow-up after excision due to the potential for malignant transformation and recurrence of poroma [1].
Conclusion
In conclusion, our report highlights the rare occurrence of EP in the breast. Despite its rarity, EP should be considered in the differential diagnosis of a slowly growing breast mass with typical clinical features. Rigorous evaluation is essential to rule out other malignancies such as breast cancer. Treatment typically involves complete surgical excision with clear margins followed by histopathological examination and immunohistochemical staining for confirmation.
EP has an excellent prognosis with low rates of recurrence or malignant transformation, however eccrine porocarcinoma should be considered as a potential outcome.
Consent
A consent was obtained from the patient to publish this case report and accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal on request.
Ethical Approval
This case report is exempt from ethical approval in our institute. Case reports are exempt from ethical approval in our university hospital.
Conflict of Interest Statement
The authors declare that they have no competing interests relevant to the content of this article.
References
- Wang Y, Liu M, Zheng Y, Feng Y (2021) Eccrine poroma presented as spindle-shaped plaque. Medicine (Baltimore) 100: e25971.
[Crossref], [Google Scholar], [Indexed]
- Eirini K, Christina F, Christina K, Myrto-Georgia T, Anastasia T, et al. (2023) Eccrine poroma: Pathogenesis, new diagnostic tools and association with porocarcinoma-a review. Diagnostics (Basel) 13: 2689.
[Crossref], [Google Scholar], [Indexed]
- Lim GH, Rashid FA, Wong A (2019) Eccrine poroma of the nipple: The first reported case. BMJ Case Rep 12: e228665.
[Crossref], [Google Scholar], [Indexed]
- Jan NA, Masood S (2024) Poroma. StatPearls, Treasure Island.
- Azma A, Tawfik O, Casparian JM (2001) Apocrine poroma of the breast. Breast J 7: 195-198.
[Crossref], [Google Scholar], [Indexed]
- Sohrabi C, Ginimol M, Nicola M, Ahmed K, Thomas F (2023) The SCARE 2023 guideline: Updating consensus surgical case report (SCARE) guidelines. Int J Surg 109: 1136-1140.
[Crossref], [Google Scholar], [Indexed]
- Fierro-Arias L, Calderón L, Peniche-Castellanos A, Mercadillo-Pérez P (2015) Periungual eccrine poroma. J Cutan Med Surg 19: 84-86.
[Crossref], [Google Scholar], [Indexed]
- Marchetti MA, Marino ML, Virmani P, Dusza SW, MarghoobAA, et al., (2018) Dermoscopic features and patterns of poromas: A multicenter observational case-control study conducted by the International Dermoscopy Society (IDS). J Eur Acad Dermatol Venereol 32: 1263-1271.
[Crossref], [Google Scholar], [Indexed]
- Choi BH, Kim MY, Lim SD, Yang JH, Ha JY, et al. (2018) Mammographic and ultrasound findings in poroid hidradenoma of the breast mimicking intraductal papilloma and papillary carcinoma: A case report. Medicine (Baltimore) 97: e11154.
[Crossref], [Google Scholar], [Indexed]
- Sawaya JL, Khachemoune A (2014) Poroma: A review of eccrine, apocrine and malignant forms. Int J Dermatol 53: 1053-1061.
[Crossref], [Google Scholar], [Indexed]
- Ma H, Liao M, Qiu S, Lu R, Lu C (2015) Eccrine poroma and porocarcinoma on the same unusual location: report on two cases. An Bras Dermatol 90: 69-72.
[Crossref], [Google Scholar], [Indexed]
- Li YX, Gudi M, Yan Z (2022) Primary eccrine porocarcinoma of the breast: A case report and review of literature. Case Rep Oncol Med 2022: 4042298.
[Crossref], [Google Scholar], [Indexed]
- Monten C, Berwouts J, Veldeman L, Creytens D, Braems G (2017) A Case of Eccrine Porocarcinoma, Located in the Breast: The Pitfalls Reviewed. Med Case Rep 4: 1-4.
[Crossref], [Google Scholar]
- Seretis K, Bounas N, Lampri E, Lykoudis EG (2022) Eccrine porocarcinoma of the face is a great imitator with aggressive behaviour. Dermatol Pract Concept 12: e2022085.
[Crossref], [Google Scholar], [Indexed]
- Jilse J, Khaylen M, Nick JL, van Bodegraven B, Vernon S, et al. (2022) Porocarcinoma: A review. Clin Exp Dermatol 47: 1030-1035.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences