Undiagnosed Preeclampsia in a Woman with Eclampsia
Kimura K, Morikawa M, Ishikawa S, Yamada T, Kojima T and Minakami H
Kimura K, Morikawa M, Ishikawa S, Yamada T, Kojima T and Minakami H*
Department of Obstetrics, Hokkaido University Graduate School of Medicine, Sapporo, Japan
- *Corresponding Author:
- Minakami H
Department of Obstetrics, Hokkaido University Graduate School of Medicine
N14 W6, Kita-ku, Sapporo 060-8638, Japan
Tel: +0353876547398
E-mail: minasho@med.hokudai.ac.jp
Received date: May 12, 2016; Accepted date: June 20, 2016; Published date: June 27, 2016
Citation: Kimura K, Morikawa M, Ishikawa S, et al. Undiagnosed Preeclampsia in a Woman with Eclampsia. Crit Care Obst & Gyne. 2016, 2:3. doi: 10.2176 7/2471-9803.100025
Copyright: © 2016 Kimura K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Keywords
Eclampsia review; Eclampsia risk; Convulsion
Introduction
Eclampsia is a serious complication occurring in 1% - 2% of women with severe preeclampsia and in 2.7-3.3 of 10,000 women [1-4]. Although the recognition and treatment of preeclampsia should theoretically eliminate eclampsia, this remains a substantial threat to maternal and fetal well-being, raising questions regarding whether the risk of eclampsia can be reduced by earlier diagnosis and treatment of preeclampsia. In Sweden, the incidence of eclampsia increased significantly from 1.5 to 3.3 per 10,000 pregnancies between 1976-1980 and 1991-1992 [2]. In the UK, only 48% of women exhibited established hypertension (diastolic BP > 90 mmHg) in the week before their first fit [4]. In 2005-2009 in Japan, one third of women with eclampsia were not recognised to have hypertension before their first fit [5]. The interval after actual onset of preeclampsia until the occurrence of an eclamptic fit is suggested short enough to prevent an eclamptic fit in some patients with eclampsia [6].
A diagnosis of preeclampsia is usually made in women developing both hypertension and significant proteinuria in pregnancy (SPIP). Proteinuria alone (not accompanied by hypertension) is detected before the first eclamptic fit in some patients with eclampsia [3,4]. As hospitalized cares are recommended to women diagnosed with preeclampsia, but not to those with hypertension alone (not accompanied by SPIP), in the UK as well as in Japan [7,8], the presence or absence of SPIP influences on clinical practice. Therefore, early detection of SPIP may be clinically important and the use of spot urine protein-to-creatinine ratio (P/Cr test) and threshold of 0.27 (mg/mg, corresponding to 30 mg/mmol) alternative to 24-h urine collection is currently recommended for the diagnosis of SPIP [7-9]. However, it is sometimes not easy to diagnose SPIP timely. Our case presented herein emphasized problems in diagnosis of SPIP and preeclampsia. The Hokkaido University Hospital Institutional Review Board approved this study and the patient provided signed informed consent.
Case Report
A 28-year-old nulliparous Japanese woman 160 cm in height was admitted to our hospital at gestational week (GW) 33-5/7 due to premature rupture of fetal membranes (PROM) following influenza A infection at GW 33-3/7. On admission, she was afebrile and treated conservatively with administration of anti-viral agent (zanamivir), prophylactic antibiotics (ampicillin) for intrauterine infection, and corticosteroids for fetal lung maturation. Blood test results showed high levels of C-reactive protein (CRP) and aspartate aminotransferase (AST) (Table 1).
| Gestational week | |||||
|---|---|---|---|---|---|
| 33–5/7 | 34–0/7 | 34–3/7 | 34–6/7* | PPD 3 | |
| Blood | |||||
| WBC (×103/μL) [3.6 - 9.0] | 4.6 | 15.0 | 6.6 | 5.5 | 6.4 |
| Hemoglobin (g/dL) [11.6 - 15.8] | 11.7 | 9.5 | 9.4 | 10.1 | 8.3 |
| Platelets (×109/μL) [120 - 400] | 184 | 182 | 210 | 263 | 264 |
| Antithrombin activity (%) [80 - 130] | 72 | 81 | - | 84 | 97 |
| AST (IU/L) [13 - 33] | 95 | 48 | 70 | 53 | 27 |
| LDH (IU/L) [119 - 229] | 268 | 216 | 199 | 208 | 197 |
| Uric acid (mg/dL) [2.3 - 7.0] | 4.7 | 4.8 | 4.9 | 8.1 | 4.4 |
| CRP (mg/dL) [0.00 - 0.39] | 7.6 | 3.4 | 1.2 | 0.4 | 3.2 |
| Urine | |||||
| Dipstick for protein | (-) | (-) | |||
| Protein (mg/dL)† | 14 | 15 | |||
| Creatinine (mg/dL)† | 24 | 41 | |||
AST: Aspartate Transaminase; CRP: C-reactive Protein; LDH: Lactate Dehydrogenase; PPD: Postpartum Day; WBC: White Blood Cell count; *: Day of Delivery; †: Determined postpartum in stocked urine specimens; Reference intervals are shown in square brackets.
Table 1: Results of laboratory work-up.
Blood pressure (BP) and proteinuria were monitored three times per day and twice a week (by dipstick test), respectively. She remained normotensive, with BP below 130/80 mm Hg and exhibited negative dipstick test results until the morning (at 06:00h) of GW 34-5/7 at which she was found to have hypertension showing 143/70 mm Hg for the first time after complaining of dull headache. Subsequent frequently measured BP were as follows; in the absence of antihypertensive drugs, 151/90 mmHg at 06:43h, and 147/78 mmHg at 07:42h followed by less than 140/90 mmHg until 14:52h at which 165/92 mm Hg was recorded. A sustained release tablet of 10 mg nifedipine given once at 15:00h was effective; 150/80 mmHg at 15:30h, 121/76 mmHg at 18:45h, and 104/68 mmHg at 21:00h. At 03:43h in the next morning, 21 hours after the development of hypertension, she was found to have a convulsive fit and BP of 117/76 mmHg after an emergent call by the patient for dizziness and headache suggestive of posterior reversible encephalopathy syndrome (PRES) [10], while planning the induction of labour.
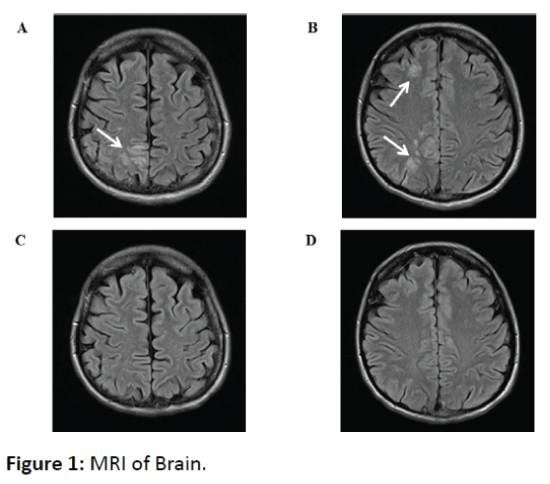
Intravenous magnesium sulphate and brain MRI given soon after the fit (Figure 1) stabilized her condition and suggested no brain hemorrhage, but PRES in this patient, respectively.
Her blood pressure remained normotensive consistently in 18-time measurement after the convulsive fit until caesarean delivery (systolic BP, 111-139 mmHg and diastolic BP, 68-83 mmHg). She gave birth to a premature, but otherwise healthy male infant weighing 2014 g with 1- and 5-min Apgar scores of 9 and 9, respectively, by emergent caesarean section 7 hours after the fit at GW 34–6/7. The neonate did not require inhaled oxygen or respiratory support, and was considered to have no congenital infection (negative CRP level in the cord blood). Her antenatal change in body weight was unremarkable (54.7 kg and 55.4 kg on days 24 and 4 prior to delivery, respectively, and 55.4 kg on the day before delivery).
Investigation
Two stocked urine specimens from this patient collected 6 days before the occurrence of the fit and on the day of the fit were later examined for protein and creatinine concentrations and revealed that the patient had already shown SPIP 6 days before the fit with a protein-to-creatinine ratio (mg/mg) > 0.27 (Table 1).
Differential diagnosis
Braine hemorrhage, brain infarct, epilepsy, and somatoform disorders were included as differential diagnoses in this patient. As brain MRI suggested PRES, eclampsia was diagnosed [10].
Outcome and follow-up
The patient remained consistently normotensive postpartum and BP ranged from 80/55 to 138/87 mmHg without medication of antihypertensive drugs. Magnesium sulphate was discontinued on postpartum day 1. Abnormal brain MRI findings on the day of the convulsion disappeared on postpartum day (PPD) 6 (Figure 1). Thus, the patient’s postpartum course was uneventful and she left the hospital on PPD 8 according to our clinical path. This patient was asymptomatic, exhibiting a body weight of 48.3 kg, BP of 100/57 mmHg, and a negative test result for urine protein on dipstick on postpartum day 43.
Discussion
The present case had preeclampsia with the duration of only 21 hours until the occurrence of an eclamptic fit. The short duration of hypertension until the eclamptic fit in this case may explain the absence of antecedent hypertension in a considerable number of women that later develop eclampsia. In addition, this case highlighted a problem inherent in dipstick testing in that false negative test results can occur in diluted urine specimens with lower creatinine concentrations [11].
Preeclampsia is usually diagnosed when women have new onset of hypertension (systolic BP ≥ 140 mm Hg and/or diastolic BP ≥ 90 mm Hg) at GW 20 or more with new onset of SPIP defined as urinary protein loss ≥ 0.3 g/day [12]. For convenience of both pregnant women and physicians, proteinto- creatinine ratio (P/Cr [mg/mg]) ≥ 0.27 in the spot urine specimen can be used as an alternative to urinary protein ≥ 0.3 g in 24-hour urine collection for diagnosis of SPIP [7-9]. The dipstick test is currently used worldwide to screen for SPIP. However, as most dipsticks for proteinuria are designed to show a positive test result with absolute protein concentration ≥ 30 mg/dL irrespective of urinary creatinine concentration and as creatinine concentrations vary greatly in spot urine specimens, e.g., from 16 mg/dL to 475 mg/dL [13], it more often shows a positive test result in concentrated urine with higher creatinine concentrations and a negative test result in diluted urine with lower creatinine concentrations [11,13]. Indeed, two urine specimens before the eclamptic fit contained relatively low creatinine concentrations (24 mg/dL and 41 mg/dL, Table 1), leading to false negative test results on two dipstick tests and delayed diagnosis of preeclampsia in this patient. This patient developed SPIP first and hypertension 5 days later. Approximately 20% to 35% of women with preeclampsia develop SPIP first, followed by hypertension later [14-16].
As this patient had been admitted due to PROM, she was retrospectively shown to have preeclampsia 21 hours before the eclamptic fit with additional P/Cr tests performed postpartum. This suggested that some preeclamptic women have a short duration of preeclampsia until the occurrence of convulsions. In a study performed in Japan in 2004, hypertension was not recognized before the eclamptic fit in 30 of 54 (56%) women with eclampsia [17]. In a detailed review of 11 eclampsia cases, hypertension was not observed until the eclamptic fit in one case, and was observed for the first time on the day of the eclamptic fit in five cases, 1 day prior to the fit in two cases, and 3, 4 and 6 days prior to the fit in one case each [6]. Thus, the time interval after diagnosis of hypertension until the eclamptic fit was within 48 hours in 73% (8/11) of cases. These results may explain why antecedent hypertension is hardly recognized in a considerable number of eclampsia women. It was speculated that some of those with a short duration of hypertension prior to the eclamptic fit may have had undiagnosed SPIP based on the present experience.
Eclampsia may be especially life-threatening if it occurs in woman while alone at home. Approximately 25-50% of women with isolated SPIP in the absence of hypertension later develop hypertension and have preeclampsia [16,18]. Therefore, accurate and prompt diagnosis of SPIP using convenient P/Cr test instead of 24-hour urine collection may contribute to better characterization of women with eclampsia. In addition, it is necessary to search for risk factors other than hypertension and SPIP for detection of women at increased risk of eclampsia. Reduced antithrombin activity and greater weight gain in the late stage of pregnancy are candidate risk factors for eclampsia [6], although the present case showed neither reduced antithrombin activity (Table 1) nor increased weight gain. Dull headache and dizziness and headache were seen shortly before hypertension onset and the convulsive fit, respectively in this patient. It was recently shown that headache and visual impairment together (60%) were most common presenting symptoms in pregnant women with PRES [10]. However, headaches are very common symptoms during pregnancy and the postpartum period with reported incidence of 39% [19].
In conclusion, this case emphasized that there are indeed women with a short duration of preeclampsia. Dipstick tests performed twice within a week before the eclamptic fit failed to detect SPIP. Urine with P/Cr of 0.27 or slightly higher is likely to be judged as negative for SPIP on dipstick test when the urine is less concentrated, as was seen in this case. To better understand eclampsia, it may be important to know that a considerable number of preeclamptic women show SPIP first and hypertension later.
References
- Sibai BM (2006) Preeclampsia as a cause of preterm and late preterm (near-term) births. In Seminars in perinatology 30: 16-19.
- Kullberg G, Lindeberg S, Hanson U (2002) Eclampsia in Sweden. Hypertension in pregnancy 21: 13-21.
- Douglas KA, Redman CWG (1994) Eclampsia in the United Kingdom. BMJ 309: 1395-1400.
- Knight M (2007) Eclampsia in the United Kingdom 2005. BJOG 114: 1072–1078.
- Morikawa M, Cho K, Yamada T, Sato S, Minakami H (2012) Risk factors for eclampsia in Japan between 2005 and 2009. Int J GynaecolObstet 117: 66-68.
- Yamada T, Kuwata T, Matsuda H, Deguchi K, Morikawa M, et al. (2012) Risk factors of eclampsia other than hypertension: pregnancy-induced antithrombin deficiency and extraordinary weight gain. Hypertension in pregnancy 31: 268-277.
- Minakami H, Maeda T, Fujii T, Hamada H, Iitsuka Y, et al. (2014) Guidelines for obstetrical practice in Japan: Japan Society of Obstetrics and Gynecology (JSOG) and Japan Association of Obstetricians and Gynecologists (JAOG) 2014 edition. J ObstetGynaecol Res 40: 1469-1499.
- NICE Clinical Guideline 107 (2010) Hypertension in Pregnancy; The Management of Hypertensive Disorders During Pregnancy.
- Côté AM, Brown MA, Lam E, von Dadelszen P, Firoz T et al. (2008) Diagnostic accuracy of urinary spot protein: creatinine ratio for proteinuria in hyper- tensive pregnant women: systematic review. BMJ 336: 1003-1006.
- Kurdoglu Z, Cetin O, SayÃÆââ¬Å¾Ãâñn R, Dirik D, Kurdoglu M et al. (2015) Clinical and perinatal outcomes in eclamptic women with posterior reversible encephalopathy syndrome. Arch GynecolObstet 292: 1013–1018.
- Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R (2010) Pre-eclampsia. The Lancet 376: 631-644.
- Baba Y, Yamada T, Obata-Yasuoka M, Yasuda S, Ohno Y, et al. (2015) Urinary protein-to-creatinine ratio in pregnant women after dipstick testing: prospective observational study. BMC Pregnancy and Childbirth 15: 331.
- Yamada T, Kojima T, Akaishi R, Ishikawa S, Takeda M, et al. (2014) Problems in methods for the detection of significant proteinuria in pregnancy. J ObstetGynaecol Res 40: 161-166.
- Akaishi R, Yamada T, Morikawa M, Nishida R, Minakami H (2014) Clinical features of isolated gestational proteinuria progressing to pre-eclampsia: retrospective observational study. BMJ Open 4: e004870.
- Sarno L, Maruotti GM, Saccone G, Sirico A, Mazzarelli LL, et al. (2015) Pregnancy outcome in proteinuria-onset and hypertension-onset preeclampsia. Hypertens Pregnancy 34: 284-290.
- Yamada T, Obata-Yasuoka M, Hamada H, Baba Y, Ohkuchi A et al. (2016) Isolated gestational proteinuria preceding the diagnosis of preeclampsia - an observational study. ActaObstetGynecol Scand.
- Minakami H, Kubo T, Takeda S, Kawabata M, Kobayashi T, et al. (2009) Placental abruption, HELLP syndrome, and Eclampsia in Japan. Nippon Sanka-FujinkaGakkaiZasshi 61: 1559-1567.
- Morikawa M, Yamada T, Yamada T, Cho K, Yamada H, et al. (2008) Pregnancy outcome of women who developed proteinuria in the absence of hypertension after mid- gestation. J Perinat Med 36: 419-424.
- Sperling JD, Dahlke JD, Huber WJ, Sibai BM (2015) The Role of Headache in the Classification and Management of Hypertensive Disorders in Pregnancy. ObstetGynecol 126: 297-302.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences