Independent Risk Factors for Postpartum Haemorrhage
Kinuko Nakagawa, Takashi Yamada, Kazutoshi Cho, Rina Akaishi, Yuko Kohgo, Kaoru Hanatani and Hisanori Minakami
Kinuko Nakagawa1, Takashi Yamada2, Kazutoshi Cho3, Rina Akaishi3, Yuko Kohgo1, Kaoru Hanatani1 and Hisanori Minakami3*
1Department of Obstetrics and Gynecology, Tomakomai City Hospital, Tomakomai, Hokkaido, Japan
2Department of Obstetrics and Gynecology, JCHO Hokkaido Hospital, Sapporo, Hokkaido, Japan
3Department of Perinatal Medicine, Hokkaido University Hospital, Sapporo, Hokkaido, Japan
- Corresponding Author:
- Hisanori Minakami
Department of Obstetrics
Hokkaido University Graduate School of Medicine
Sapporo, Hokkaido, Japan
Tel: +0353876547398
E-mail: minasho@med.hokudai.ac.jp
Received Date: March 22, 2016; Accepted Date: March 28, 2016; Published Date: April 06, 2016
Citation: Nakagawa K, Yamada T, Cho K. Independent risk factors for postpartum haemorrhage. Crit Care Obst&Gyne. 2016, 2:2. doi: 10.21767/2471-9803.100018
Copyright: © 2016 Nakagawa K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Postpartum hemorrhage (PPH) is the leading cause of maternal mortality. To evaluate the possibility that antepartum fibrinogen is associated with risk of postpartum hemorrhage.
Methods and Findings: Retrospective analysis was performed among 949 women with vaginal deliveries of singletons at gestational week (GW) ≥ 36 to examine associations of PPH, defined as estimated blood loss (EBL) ≥ 700 mL, with antepartum blood fibrinogen, platelet count, and hemoglobin levels within 7 days prior to delivery and demographic characteristics, including, parity, maternal age, pre-pregnancy body mass index, duration of labor, instrumental delivery, and birthweight. Logistic multiple regression analysis was performed to identify independent risk factors and odds ratios (OR). PPH occurred in 127 (13%) women and was less frequent as levels of fibrinogen increased with OR (confidence interval) 0.97 (0.95 – 0.99) for 1.0 g/L increase in fibrinogen level by logistic multiple regression analysis. The other independent risk factors for PPH included nulliparity,1.08 (1.03 – 1.12) and increased birthweight 1.02 (1.01 – 1.03) for each 100 g increase in birthweight. PPH was more common in nulliparous than multiparous women (16% [77/474] vs. 11% [50/475]) and in women with instrumental deliveries (27% [8/30] vs. 13% [119/919]). EBL was significantly negatively correlated with fibrinogen and hemoglobin levels and positively with GW at delivery and infant birthweight.
Conclusions: Antepartum fibrinogen level was an independent risk factor for PPH, and each 1.0 g/L decrease of antenatal fibrinogen level increased the risk of PPH by 2.9% independent of other factors.
Keywords
Blood transfusion; Fibrinogen; Pregnancy; Postpartum haemorrhage
Introduction
Fibrinogen, a positive acute-phase protein elevating in any form of inflammation as well as in pregnancy, is the soluble precursor of fibrin and a key contributor to both primary and secondary hemostasis, promoting clot formation and platelet aggregation. Patients with hypofibrinogenemia (defined as a fibrinogen level<1.5 g/L) are prone to bleeding when exposed to trauma or after giving birth [1,2]. Although fibrinogen levels differ considerably between assay methods, blood fibrinogen level increases to approximately double during pregnancy [3-6] suggesting a physiological role of increased fibrinogen level in maintaining pregnancy and postpartum hemostasis [2].
Postpartum hemorrhage (PPH) is the leading cause of maternal mortality [7] and is associated with 12.5% – 19.1% of maternal mortalities in the USA [8,9]. PPH accounted for 14.1%, 9.7%, and 6.7% of all causes of maternal mortality in Japan in 2000, 2005, and 2010, respectively [10]. Various etiologies, such as uterine rupture, uterine inversion, retained placenta, and severe birth canal injury, may be identified in some cases of PPH, but the definite etiology remains unclear in the majority of cases. Although the leading etiology of PPH is uterine atony, this is poorly defined at present and represents a diagnosis of exclusion.
Twin pregnancy is a risk factor of PPH [11,12] Uterine overdistension is considered to be attributable to PPH via uterine atony in twin pregnancy [11]. However, fibrinogen level determined at the initial stage of PPH is known to be a good predictor of subsequent severe PPH [13-16] and women with twin pregnancy are likely to exhibit a gradual decline in fibrinogen level in the last several weeks of pregnancy leading to lower antepartum fibrinogen level compared to those with singleton pregnancies [17]. These observations suggest that a low antepartum fibrinogen level may be associated with higher risk of PPH. Indeed, at least two studies suggested that lower antepartum fibrinogen level was associated with increased risk of PPH [18,19].
However, many demographic characteristics other than antepartum fibrinogen levels may influence the risk of PPH. This retrospective study was conducted to determine independent risk factors for PPH.
Materials and Methods
This retrospective study was conducted with the approval of the Ethics Committee of Tomakomai City Hospital, Tomakomai, Hokkaido, Japan.
Participants
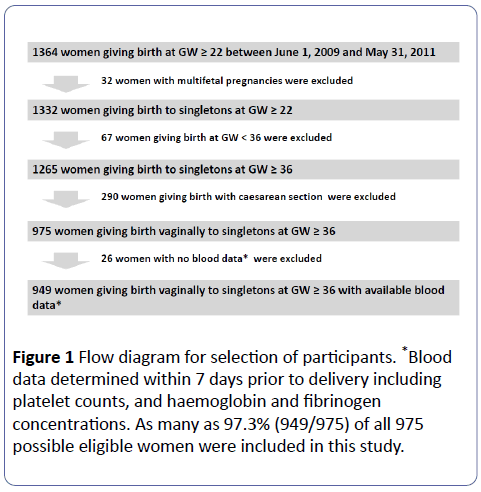
During the 2-year study period between June 1, 2009, and May 31, 2011, a total of 1265 women gave birth to singleton infants on gestational week (GW) 36 or more at Tomakomai City Hospital (TCH) (Figure 1).
Of these, 975 women (77%) gave birth vaginally. During the study period at the TCH, complete blood cell counts and blood fibrinogen concentration were determined as part of the routine laboratory work-up on admission of women for childbirth. Thus, three blood variables, i.e., fibrinogen concentration, haemoglobin (Hb) concentration, and platelet counts, were determined simultaneously in the same blood samples. All data from the institutional central laboratory regarding blood fibrinogen levels, Hb concentrations, and platelet counts determined in pregnant women were provided for this study with the patients’ names and corresponding identification number for each individual during the study period. After matching data on blood tests with medical charts, 949 women were identified as having data on blood tests determined within 7 days prior to delivery. Information on clinical and demographic characteristics was obtained from medical charts of these 949 women. Thus, 949 women accounted for 97.3% of all 975 women who gave birth to singleton infants on or after GW 36 during the study period. Blood variables were determined on the day of delivery (before delivery) in 553 (58%) women, and 1, 2, 3, 4, and 5 days before delivery in 315 (33%), 58 (6.1%), 18 (1.9%), 4 (0.4%), and 1 (0.1%) of the 949 women, respectively. Thus, more than 90% of data on blood variables were those determined within 48 hours before delivery.
Determination of fibrinogen level and definition of PPH
The fibrinogen levels were measured at the TCH using a coagulation analyzer (ACL TOP series and STACIA®; Instrumentation Laboratory, Bedford, MA, USA) and reagents provided by Mitsubishi Chemical Medience Co. Ltd. (Tokyo, Japan). The correlation of fibrinogen values (y) obtained by this system with those (x) obtained with another coagulation analyzer (CS-5100®; Sysmex Co. Ltd., Tokyo, Japan) was as follows: y = 1.4x – 4.1, R2 = 0.9648. PPH was defined as EBL ≥ 700 mL in accordance with a previous report [18].
Statistical Analysis
Data are presented as medians. Statistical analyses were performed using the JMP10© statistical software package (SAS, Cary, NC, USA). Fisher’s exact probability test was used for comparison of categorical variables. The Wilcoxon/Kruskal– Wallis method was used for comparison of medians. Logistic multiple regression analysis with a stepwise procedure (a significance level of 0.1 was required to allow a variable into the model, and a significance level of 0.05 was required for a variable to stay in the model) was performed to identify independent predictors of PPH and determine the odds ratios (OR) using IBM SPSS Statistics® (ver. 19.0, IBM Japan Service Co. Ltd., Tokyo, Japan). In all analyses, P < 0.05 was taken to indicate statistical significance.
Results
The median EBL was 312 mL and EBL ≥ 500 mL, ≥700 mL, ≥800 mL, ≥1000 mL, and ≥1500 mL occurred within 24 hours after delivery in 214 (22.6%), 127 (13.3%), 98 (10.3%), 57 (6.0%), and 22 (2,3%) of the 949 women, respectively (Table 1). Thus, PPH occurred in 13.3% of the 949 women in this study. In comparison with 822 women without PPH (Table 1), the numbers of nulliparous women and of women with instrumental delivery were significantly greater, antepartum levels of Hb and fibrinogen were significantly lower, GW at delivery was significantly more advanced, and infant birthweight was significantly greater in 127 women with PPH. Characteristics of nulliparous women and women with instrumental delivery (Table 2).
| EBL (mL) | ||||
| Overall | <700 | ≥700 | P-value | |
| Number of women | 949 | 822 | 127 | 0.8606 |
| Age (years) | 29 (16 - 45) | 29 (16 - 44) | 29 (18 - 45) | 0.0097 |
| Nulliparity | 474 (50.0%) | 397 (48.3%) | 77 (60.6%) | 0.8092 |
| Pre-pregnancy BMI (kg/m2) | 20.5 (14.4 –1.5) | 20.6 (14.4 – 41.5) | 20.5 (16.4 – 35.2) | 0.0135 |
| Hemoglobin concentration (g/dL) | 10.9 (7.4 – 6.5) | 10.9 (7.4 – 16.5) | 10.6 (8.2 – 14.8) | 0.0728 |
| Platelet count (×109/L) | 23.6 (4.5 – 8.5) | 23.8 (4.5 – 48.5) | 22.8 (9.4 – 40.4) | 0.0421 |
| Fibrinogen concentration (mg/dL) | 538 (295 - 147) | 540 (295 - 1147) | 524 (331 - 894) | 0.0001 |
| GW at delivery | 39.6 (36.1 – 1.9) | 39.6 (36.1 – 41.9) | 39.9 (36.6 – 1.9) | 0.2461 |
| Duration of labor (min) | 380 (29 - 2385) | 376 (29 - 2385) | 409 (43 - 2152) | 0.0369 |
| Operative delivery | 30 (3.2%) | 22 (2.7%) | 8 (6.3%) | <0.0001 |
| Infant birth weight (g) | 3040 (1642 - 4220) | 3015 (1642 - 4220) | 3195 (2106 - 4045) | 0.7467 |
| Male infant | 488 (51.4%) | 421 (51.2%) | 67 (52.8%) | <0.0001 |
| EBL (mL) | 312 (50 - 3900) | 282 (50 - 691) | 940 (700-3900) | <0.0001 |
| ≥500 | 214 (22.6%) | 87 (10.6%) | 127 (100%) | <0.0001 |
| ≥700 | 127 (13.4%) | 0 (0.0%) | 127 (100%) | <0.0001 |
| ≥800 | 98 (10.3%) | 0 (0.0%) | 98 (77.2%) | <0.0001 |
| ≥1000 | 57 (6.0%) | 0 (0.0%) | 57 (44.9%) | <0.0001 |
| ≥1500 | 22 (2.3%) | 0 (0.0%) | 22 (17.3%) | 0.8606 |
Table 1: Demographic characteristics of participants.
| Nulliparity | Instrumental delivery | |||
| Yes (n=474) | No (n=475) | Yes (n=30) | No (n=919) | |
| Nulliparity | NA | NA | 28 (93%) | 446 (49%)* |
| GW at delivery | 39.6 | 39.4* | 39.7 | 39.6 |
| Birth-weight (g) | 3000 | 3085* | 3121 | 3040 |
| Instrumental delivery | 28 (5.9%) | 2 (0.4%)* | NA | NA |
| Hemoglobin (g/dL) | 11.1 | 10.7* | 10.9 | 10.9 |
| Platelet (×109/L) | 22.8 | 24.5* | 22.3 | 23.6 |
| Fibrinogen (g/L) | 5.40 | 5.37 | 5.17 | 5.39 |
| EBL (mL) | 330 | 290* | 461 | 310* |
| PPH | 77 (16%) | 50 (11%)* | 8 (27%) | 119 (13%)* |
Table 2: Association of nulliparity and instrumental delivery with other variables.
Nulliparous women gave birth to significantly smaller infants, had significantly higher rates of instrumental delivery, exhibited significantly higher antepartum Hb levels and greater EBL, and had significantly higher rates of PPH compared to multiparous women.
Women with instrumental delivery were significantly more likely to be nulliparous, exhibited greater EBL, and had significantly higher rates of PPH compared to those who gave birth without the aid of instruments. Fibrinogen levels did not differ significantly between two groups divided by either prior history of childbirth or the use of instruments in the current childbirth.
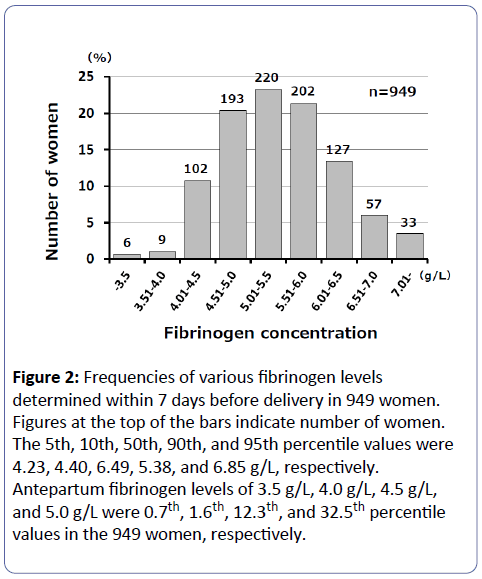
Distribution of antepartum fibrinogen levels (Figure 2). Antepartum fibrinogen concentrations of ≤4.0 g/dL, 4.01-4.5 g/L, and 4.51-5.0 g/L were seen in 1.6% (15/949), 11% (102/949), and 20% (193/949) of the 949 women, respectively (Figure 2).
Figure 2: Frequencies of various fibrinogen levels determined within 7 days before delivery in 949 women. Figures at the top of the bars indicate number of women. The 5th, 10th, 50th, 90th, and 95th percentile values were 4.23, 4.40, 6.49, 5.38, and 6.85 g/L, respectively. Antepartum fibrinogen levels of 3.5 g/L, 4.0 g/L, 4.5 g/L, and 5.0 g/L were 0.7th, 1.6th, 12.3th, and 32.5th percentile values in the 949 women, respectively.
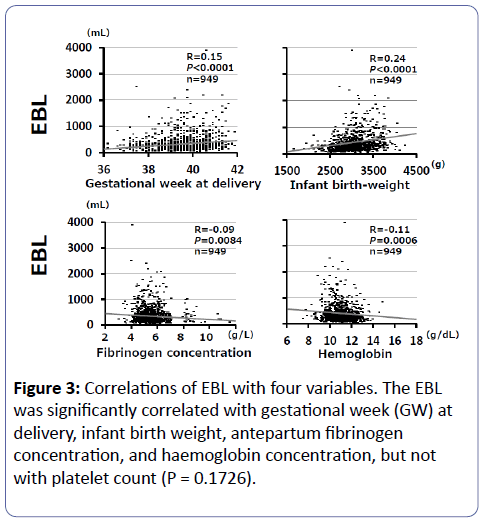
Correlations of EBL with GW at delivery, infant birthweight, and antepartum fibrinogen and Hb levels (Figure 3).
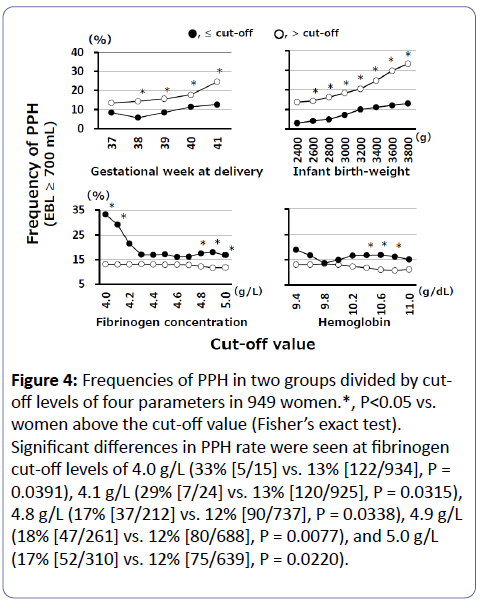
The EBL showed significant positive correlations with GW at delivery (P<0.0001) and infant birthweight (P<0.0001), and significant negative correlations with fibrinogen level (P = 0.0084) and Hb level (P = 0.0006) (Figure 3), but not with platelet count (P = 0.1726). Thus, women with advanced GW at delivery, greater infant birthweight, lower antepartum fibrinogen level, and lower antepartum Hb level were suggested to be at higher risk of PPH. Indeed, the prevalence rate of PPH differed significantly between two groups divided by certain cut-off values of GW at delivery, infant birthweight, antepartum fibrinogen level, and antepartum Hb level (Figure 4). An effect of small-for-gestational age (SGA) infant on PPH was examined separately. The PPH occurred significantly less often in the SGA cases than in the remaining cases not having SGA (2.5% [2/79] vs. 14.4% [125/870], P = 0.0007).
Figure 4: Frequencies of PPH in two groups divided by cutoff levels of four parameters in 949 women.*, P<0.05 vs. women above the cut-off value (Fisher’s exact test). Significant differences in PPH rate were seen at fibrinogen cut-off levels of 4.0 g/L (33% [5/15] vs. 13% [122/934], P = 0.0391), 4.1 g/L (29% [7/24] vs. 13% [120/925], P = 0.0315), 4.8 g/L (17% [37/212] vs. 12% [90/737], P = 0.0338), 4.9 g/L (18% [47/261] vs. 12% [80/688], P = 0.0077), and 5.0 g/L (17% [52/310] vs. 12% [75/639], P = 0.0220).
Independent Risk Factors for PPH
The following seven factors were entered into the model: nulliparity (yes/no), instrumental delivery (yes/no), and continuous variables of GW at delivery, infant birthweight, Hb, platelet count, and fibrinogen level. Three factors, i.e., nulliparity, infant birthweight, and fibrinogen level, were selected as significant independent risk factors for PPH. The OR (95% confidence interval) were 1.08 (1.03 – 1.12) for nulliparity (P<0.001), 1.02 (1.01 – 1.03) for each 100 g increase in birthweight (P<0.001), and 0.97 (0.95 – 0.99) for each 1.0 g/L increase in fibrinogen level (P = 0.013). Thus, nulliparous women had a 1.08-fold higher risk of PPH independent of other factors, and each 100 g increase in birthweight and 1.0 g/L decrease in antepartum fibrinogen level increased the risk of PPH by 2.0% and 2.9%, respectively, independent of other factors.
Discussion
This study indicated that antepartum fibrinogen level as well as nulliparity and infant birth weight were independent risk factors for PPH.
Fibrinogen level determined during PPH has been identified as an important factor influencing the clinical course of PPH [13-16] Women that developed severe PPH later had a low fibrinogen level at the initial stage of PPH [13-16] fibrinogen determined at the initial stage of PPH is the only marker associated with the occurrence of severe PPH [14-16] and the risk of severe PPH increases by 2.63-fold for each 1.0 g/L decrease in fibrinogen level determined at the initial stage of PPH [14]. These previous reports indicated that fibrinogen level at the initial stage of PPH is a significant predictor of the severity of PPH, and decreases in fibrinogen level are well correlated with EBL during PPH. In addition, these reports also suggested that antenatal fibrinogen level before commencement of labor may be lower for women who will develop PPH than for those who will not develop PPH, i.e., a low antepartum fibrinogen level is a risk factor for the occurrence of PPH.
This was true in at least three different cohorts [18,19] including the present study: mean (SD) or median antepartum fibrinogen level was significantly lower for PPH than for non- PPH women with vaginal deliveries, i.e., 4.3 (1.3) vs. 4.9 (1.0) g/L, respectively (P<0.05), in a study by Simon et al. [19] 3.93 vs. 4.18 g/L, respectively (P = 0.025), in a study by Yamada [18], and 5.2 vs. 5.4 g/L, respectively (P = 0.0421), in the present study (Table 1); and the relative risk of PPH was 6.09 (3.30 – 11.25) (35% [9/26] vs. 5.9% [37/651], respectively) for women with <3.8th percentile fibrinogen value (2.9 g/L) in the study by Simon et al. [19] 2.01 (1.20 – 3.39) (38% [11/29] vs. 19% [58/308], respectively) for women with <8.3rd percentile fibrinogen value (3.3 g/L) in the study by Yamada et al. [18] and 2.25 (1.17 – 4.28) (29% [7/24] vs. 13% [120/925], respectively) for women with ≤2.5th percentile fibrinogen value (4.1 g/L) in the present study (Figure 4). Thus, women with a low antepartum fibrinogen value had significantly higher risks of PPH compared to those without a low antepartum fibrinogen value in these three studies. However, in a study by Peyvandi [20] the mean fibrinogen level was similar between women with and without PPH of EBL ≥ 500 mL (4.8 g/L vs. 4.8 g/L, respectively) and the PPH prevalence rate was similar between quintiles according to antepartum fibrinogen levels (25%, 25%, 24%, 24%, and 23% for the 1st, 2nd, 3rd, 4th, and 5th quintile groups, respectively). The corresponding values in the present study were 27%, 24%, 24%, 21%, and 17%, respectively, if we stratified the 949 women according to ascending antepartum fibrinogen level quintiles and used EBL ≥ 500 mL as a definition of PPH.
The following observations may further support our finding that antepartum fibrinogen is a risk factor for PPH; the prevalence rate of low fibrinogen level (<2.0 g/L) determined 6 – 9 months after delivery was reported to be more frequent in women that had experienced severe PPH than in those who had not (8.1% [28/347] vs. 2.5% [16/634], respectively) and a low fibrinogen level 6 – 9 months after delivery was shown to be independently associated with a significant risk of severe PPH [21]. It was speculated that women with low postpartum fibrinogen level 6 – 9 months after delivery would have exhibited an insufficient fibrinogen increase during pregnancy, thus leading to a low antepartum fibrinogen level and elevated risk of PPH.
The absolute fibrinogen values differed considerably between studies, possibly due to differences in assay methods used; 50th percentile fibrinogen value was 4.9 g/L in the study by Simon et al. [19] mean antepartum fibrinogen level was 4.8 g/L in that by Peyvandi et al. [20], 20th and 50th percentile fibrinogen values were 3.60 and 4.11 g/L in the study by Yamada et al. [18] and the 10th and 50th percentile fibrinogen values were 4.4 and 5.38 g/L in the present study. Therefore, although the absolute fibrinogen values were higher compared to those in studies by Yamada et al.18 and Simon et al. [19] they were relatively similar to those in two other studies in which 2.5th – 97.5th percentile values were 3.5 – 6.5 g/L (10.3 – 19.1 μmol/L) at GW 35 – 424 and mean value was 5.2 g/L (15.4 μmol/L) at GW 34 – 37 in another [5].
Macrosomia and instrumental delivery, but not nulliparity, were listed as risk factors for PPH [11,22]. In a recent study by Prick et al. [23] severe PPH defined as EBL ≥ 1000 mL was shown to occur in approximately 5.0% of Danish women, and the risk of severe PPH increased with increasing infant birth weight: 3.5%, 4.2%, and 6.8% for spontaneous vaginal deliveries of infants with birth weight<10th percentile, 10 – 90th percentile, and >90th percentile, respectively, and was more common in nulliparous than multiparous women (5.1% vs. 3.9%, respectively) and in women with assisted vaginal delivery than spontaneous vaginal delivery (6.4% vs. 4.3%, respectively) [23] consistent with the results of the present study. In the UK population, the most severe PPH defined as EBL ≥ 1500 mL occurs in 2.8% (74/2608) and 1.3% (121/9453) of women with instrumental and spontaneous vaginal deliveries, respectively [15]. However, nulliparous women accounted for 93% (28/30) of those with instrumental deliveries, and instrumental deliveries were used more often in nulliparous than in multiparous women (5.9% vs. 0.4%, respectively) (Table 2), and nulliparity, but not instrumental delivery was an independent risk factor for PPH in this study. Thus, instrumental delivery was a confounding factor in this study.
Although PPH is usually defined as EBL ≥ 500 mL [24] this study defined PPH as EBL ≥ 700 mL, which occurred in 13% (127/949) of women with vaginal singleton deliveries, based on the following observations: EBL ≥ 500 mL is common, occurring in 42% of Japanese women with vaginal deliveries, [18] in 24% of 4061 Italian women with vaginal deliveries [20] and in 23% of the 949 women in this study; and the Japanese Guidelines for Obstetrical Practice report a 90th percentile value of EBL after vaginal delivery of 800 mL [25] In the Danish population, although PPH defined as EBL ≥ 500 mL is less common, occurring in 12% (429/3521) of singleton pregnancies, including caesarean deliveries [26] compared to 23% (214/949) in this study, severe PPH defined as EBL ≥ 1000 mL occurs in approximately 5.0% of women with vaginal deliveries,23 comparable to that of 6.0% (59/949) in this study. In the UK population, EBL ≥ 1500 mL occurs in 1.6% of women with vaginal deliveries [15] comparable to the value of 2.3% in this study (Table 1). Thus, the prevalence rate of EBL around 500 mL differed considerably between study populations, but its rate around 1000 mL or more did not differ markedly between study populations.
Our results may not have been distorted by the retrospective cohort study design as our protocol for management of pregnant women did not include any specific treatment options according to antepartum fibrinogen level. Therefore, it was reasonable to speculate that the management of parturient women did not differ between those with low and high fibrinogen levels. In addition, as this study included 97.3% (949/975) women who gave birth to singleton infants on or after GW 36 during the study period, possible selection bias was unlikely to have affected the results.
In conclusion, the present study including 949 women (97.3% of all possible eligible women) demonstrated that antepartum fibrinogen level as well as nulliparity and infant birth weight are independent risk factors for PPH (defined as EBL ≥ 700 mL, occurring in 13% of women). Nulliparous women had a 1.08-fold higher risk of PPH independent of other factors, and each 100 g increase in birth weight and each 1.0 g/L decrease of antepartum fibrinogen level increased the risk of PPH by 2.0% and 2.9%, respectively, independent of other factors.
Acknowledgement
We thank the staff of the Department of Obstetrics and Gynecology, Tomakomai City Hospital, for their cooperation in blood sampling.
Disclosure
The authors have no conflicts of interest to declare.
References
- Peyvandi F (2012) Epidemiology and treatment of congenital fibrinogen deficiency. Thromb Res 130S2: S7-S11.
- Kaparou M, Danilatou V, Lydaki E, Stathoudakis G, Bolonaki I, et al. (2012) Prophylactic administration of fibrinogen concentrate in a pregnant woman with congenital hypofibrinogenemia and a positive obstetric history of severe bleeding in previous cesarean section. Blood Coagul Fibrin 23: 566-568.
- Hui C, Lili M, Libin C, Rui Z, Fang G, et al. (2012) Changes in coagulation and hemodynamics during pregnancy: a prospective longitudinal study of 58 cases. Arch Gynecol Obstet 285: 1231-1236.
- Szecsi PB, Jørgensen M, Klajnbard A, Andersen MR, Colov NP, et al. (2010) Haemostatic reference intervals in pregnancy. Thromb Haemos 103: 718-727.
- Hansen AT, Andreasen BH, Salvig JD, Hvas AM (2011) Changes in fibrin D-dimer, fibrinogen, and protein S during pregnancy. Scand J Clin Lab Invest 71: 173-176.
- Liu J, Yan E, Lee L (2012) Gestational age-specific reference intervals for routine haemostatic assays during normal pregnancy. Int J Clin Chem 413: 258-261.
- Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF (2006) WHO analysis of causes of maternal death: a systematic review. Lancet 367: 1066-1074.
- Bateman BT, Berman MF, Riley LE, Leffert LR (2010) The epidemiology of postpartum hemorrhage in a large, nationwide sample of deliveries. Anesth Analg 110: 1368-1373.
- Berg CJ, Callaghan WM, Syverson C, Henderson Z (2010) Pregnancy-related mortality in the United States, 1998 to 2005. Obstet Gynecol 116: 1302-1309.
- Mother’s & Children’s Health & Welfare Association (2011) Maternal and child health statistics of Japan. Mother’s & Children’s Health Organization. Tokyo, Japan.
- ACOG Practice Bulletin, No. 76. Postpartum hemorrhage (2006) Obstet Gynecol 108: 1039-1047.
- Suzuki S, Hiraizumi Y, Miyake H (2012) Risk factors for postpartum hemorrhage requiring transfusion in cesarean deliveries for Japanese twins: comparison with those for singletons. Arch Gynecol Obstet 286: 1363-1367.
- Gayat E, Resche-Rigon M, Morel O, Rossignol M, Mantz J, et al. (2011) Predictive factors of advanced interventional procedures in a multicentre severe postpartum haemorrhage study. Intensive Care Med 37: 1816-1825.
- Charbit B, Mandelbrot L, Samain E, Baron G, Haddaoui B, et al. (2007) The decrease of fibrinogen is an early predictor of the severity of postpartum hemorrhage. J Thromb Haemost 5: 266-273.
- De Lloyd L, Bovington R, Kaye A, Collis RE, Rayment R, et al. (2011) Standard haemostatic tests following major obstetric haemorrhage. Int J Obstet Anesth 20: 135-141.
- Cortet M, Deneux-Tharaux C, Dupont C (2012) Association between fibrinogen level and severity of postpartum haemorrhage: secondary analysis of a prospective trial. Br J Anaesth 108: 984-989.
- Yamada T, Morikawa M, Yamada T, Akaishi R, Kojima T, et al. (2015) Fibrinogen levels in the late stage of twin pregnancy. Thromb Res 135: 318-321.
- Yamada T, Akaishi R, Oda Y, Nishida R, Yamada T, et al. (2014) Antenatal fibrinogen concentrations and postpartum haemorrhage. Int J Obstet Anesth 23: 365-370.
- Simon L, Santi TM, Sacquin P, Hamza J (1997) Pre-anaesthetic assessment of coagulation abnormalities in obstetric patients; usefulness, timing and clinical implications. Br J Anaesth 78: 678-683.
- Peyvandi F, Biguzzi E, Franchi F, Bucciarelli P, Acaia B, et al. (2012) Elevated prepartum fibrinogen levels are not associated with a reduced risk of postpartum hemorrhage. J Thromb Hemos 10: 1451-1453.
- Chauleur C, Cochery-Nouvellon E, Mercier E, Aya G, Fabbro-Peray P, et al. (2008) Some hemostasis variables at the end of the population distributions are risk factors for severe postpartum hemorrhages. J Thromb Haemos 6: 2067-2074.
- Wikkelsø AJ (2015) The role of fibrinogen and haemostatic assessement in postpartum haemorrhage. Dan Med J 61: B5055.
- Prick BW, Auf Altenstadt JF, Hukkelhoven CW, Bonsel GJ, Steegers EA, et al. (2015) Regional differences in severe postpartum hemorrhage: a nationwide comparative study of 1.6 million deliveries. BMC Pregnancy Childbirth 15: 43.
- WHO Guidelines for the Management of Postpartum Haemorrhage and Retained Placenta.
- Japan Society of Obstetrics and Gynecology and Japan Assocciation of Obstetricians and Gynecologists. Guidelines for Obstetrical Practice in Japan: Japan Society of Obstetrics and Gynecology (JSOG) and Japan Association of Obstetricians and Gynecologists (JAOG) 2011 edition (in Japanese). Japan Society of Obstetrics and Gynecology.
- Wise LA, Mikkelsen EM, Sørensen HT, Rothman KJ, Hahn KA, et al. (2015) Prospective study of time to pregnancy and adverse birth outcomes. Fertil Steril 103: 1065-1073.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences