The Great Masquerader: Paraganglioma Diagnosed in the Third Trimester of Pregnancy
Vi Duong1*, Alison Gambou2, Rebecca Chornock1, Sara Iqbal3 and Elizabeth Coviello4
1Department of Obstetrics and Gynecology, Georgetown University, Washington, USA
2Department of Obstetrics and Gynecology, Newark Beth Israel Medical Center, Newark, USA
3Department of Obstetrics and Gynecology, Medstar Washington Hospital Center, Washington, USA
4Department of Obstetrics and Gynecology, University of North Carolina-Chapel Hill, Chapel Hill, USA
- *Corresponding Author:
- Vi Duong
Department of Obstetrics and Gynecology,
Georgetown University,
Washington,
USA;
Email: viduong414@gmail.com
Received: May 15, 2020 Manuscript No. IPCCO-23-4119; Editor assigned: May 18, 2020, PreQC No. IPCCO-23-4119 (PQ); Reviewed: May 21, 2020, QC No. IPCCO-23-4119; Revised: November 8, 2023, Manuscript No. IPCCO-23-4119 (R); Published: December 6, 2023, DOI: 10.36648/2471-9803.9.6.138
Citation: Duong V, Gambou A, Chornock R, Iqbal S, Coviello E (2023) The Great Masquerader: Paraganglioma Diagnosed in the Third Trimester of Pregnancy. Crit Care Obst Gyne Vol.9 No.6:138.
Abstract
Background: Paragangliomas are rare neuroendocrine tumors located outside the adrenal gland. Diagnosis is often delayed because clinical symptoms mimic preeclampsia or gestational hypertension. Controversy exists on immediate or interval tumor removal diagnosed in the third trimester. Guidelines lack regarding surgical cesarean delivery technique and obstetrical considerations for tumor excision at time of delivery.
Case presentation: A 17-year-old at 30 weeks gestation presented with hypertensive emergency and diagnosed with preeclampsia. Further evaluation revealed a paraganglioma. She was treated with alpha blockade prior to a planned cesarean delivery at 34 weeks with concomitant tumor excision. The procedure was complicated by aortic laceration, uterine atony, profound hypotension and DIC.
Conclusion: Not all cases of severe hypertension are preeclampsia. Secondary causes of hypertension in an adolescent during pregnancy should be considered. Preoperative management with alpha blockade presents a challenge for treatment of hemorrhagic shock and DIC. A multidisciplinary approach is essential to reduce morbidity. Women diagnosed with paraganglioma and their neonates should be offered genetic counseling.
Keywords
Paragangliomas; Pregnancy; Preeclampsia; Adolescent
Introduction
Pheochromocytomas and Paragangliomas (PPGLs) are rare neuroendocrine tumors that are derived from chromaffin cells in the adrenal medulla or extraadrenal sympathetic ganglia, respectively. The incidence of these tumors is <0.2 in 10,000 pregnancies (0.002%). If undiagnosed, maternal and fetal mortality can be 50%. Commonly, gravid women presenting in hypertensive urgency or emergency are considered to have preeclampsia, delaying the diagnosis of alternative etiologies of hypertension including PPGLs. The body of literature for PPGLs in pregnancy is mainly case reports. Guidelines lack regarding surgical cesarean delivery technique and obstetrical considerations for tumor excision at time of delivery [1].
Case Presentation
A 17-year-old African American, primigravida at 30 weeks gestational age presented with complaints of chest pain, shortness of breath and hypertensive emergency with blood pressure 212/120 mmHg. Her history included chronic hypertension diagnosed at age 16, an Amplatzer repair of an atrial septal defect in 2006 and asthma. Her presentation was concerning for preeclampsia with severe features and she was started on magnesium therapy and received labetalol and betamethasone. Her blood pressures quickly stabilized, preeclampsia labs were normal and magnesium therapy was discontinued. Labs and imaging studies ordered for evaluation of secondary causes of hypertension included a normal echo and urine normetanephrines. Prior to results of the urine studies, she signed out against medical advice [2].
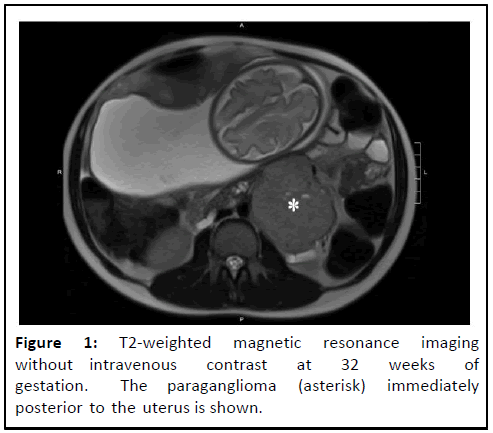
At 32 weeks gestational age, she presented to clinic with persistently severe range blood pressure (156/101 mmHg, 161/108 mmHg). She was noted to have markedly elevated normetanephrines at 19.370 mcg/gm (normal range: 0 mcg/ gm-450 mcg/gm) from her prior admission. She was admitted for blood pressure management and the endocrine team recommended thyroid antibodies, 24 hr urine metanephrines, salivary cortisol testing, aldosterone/renin ratio, bilateral renal ultrasound and abdominal MRI. On MRI, an 8 cm left infrarenal mass consistent with extraadrenal paraganglioma was visualized (Figure 1) [3].
Comprehensive laboratory tests, including intact Parathyroid Intact Hormone (PTH) and thyroid antibodies (TPO, TSI, TRAB) plasma metanephrines level, plasma normetanephrines, plasma epinephrine, fractionated dopamine and fractionated norepinephrine, were significant for an elevated plasma normetanephrines at greater than 50 (normal 0.00 nmol/L-0.89 nmol/L), a significantly elevated fractionated plasma norepinephrine of 18,977 (normal range: 85 pg/ml-1250 pg/ml) and an elevated fractionated dopamine of 83 (normal range: 0 pg/ml-20 pg/ml). Prior to delivery and surgery, she had genetic screening, which showed a Succinate Dehydrogenase, subunit B (SDHB) mutation, which is associated with autosomal dominant pheochromocytoma/paraganglioma syndrome [4].
Upon diagnosis, she was started on oral phenoxybenzamine with goal to titrate medication to orthostasis. This presented a challenge for placental perfusion and the goal was altered to systolic blood pressure <140 and heart rate <110. Phenoxybenzamine was initiated at 10 mg twice daily. Rate control was achieved with oral labetalol and metoprolol. During this period, social services and ethics committee were consulted due to patient threatening to leave. Despite these services, the patient signed out against medical advice for 4 days with reported compliance on phenoxybenzamine. Upon her readmission, phenoxybenzamine was restarted and titrated to 30 mg twice daily over 10 days. On ultrasound 14 days before surgery, the estimated fetal weight was 1837 grams at the twentieth percentile with normal dopplers. Fetal status via nonstress testing was persistently reassuring in the preoperative period. After central line placement in the operating room, delivery was expedited due to fetal bradycardia once general anesthesia was established. A midline vertical skin incision was performed and a low transverse uterine incision was made for the breech delivery of a cephalic presenting, healthy female weighing 2040 grams with Apgars 5/7 at 34 weeks 5 days gestational age. No fundal pressure was employed. The hysterotomy was closed with excellent uterine tone and hemostasis. Quantitative blood loss following hysterotomy closure was 200 ml [5].
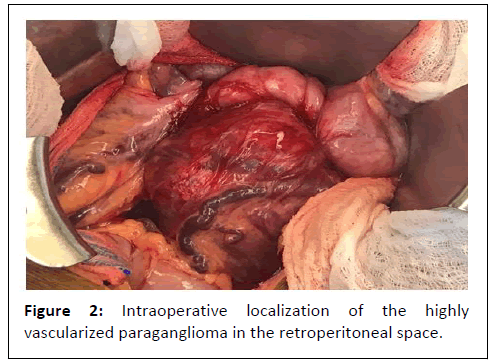
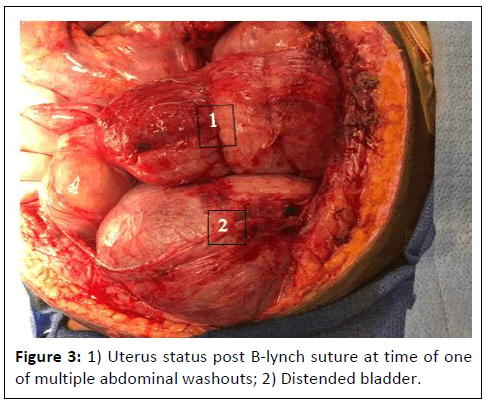
Endocrine surgery placed a Bookwalter retractor and obtained adequate visualization of the mass, including packing the uterus out of the pelvis and under the retractor. The tumor was hypervascularized and densely adherent to the aorta extending from below the aortic bifurcation to the left renal vessels. Surgical complications included an aortic laceration at the level of the inferior mesenteric artery, tumor capsular rupture during its mobilization and an unanticipated hemicolectomy with temporary colostomy formation due to tumor adhesion, which were repaired by vascular and colorectal surgery, respectively. Approximately 5 hours into the case, there was massive hemorrhage from the aortic laceration with an estimated blood loss of 2000 ml. The patient became coagulopathic and the uterus appeared atonic ballooning under the retractor with 1000 ml of blood loss noted on the floor. The massive transfusion protocol was initiated. Once the aortic laceration was repaired, 1000 ml of blood was evacuated from the uterus manually and with dilation and curettage followed by B-lynch suture. Patient received tranexamic acid, two doses of intramuscular methergine, intramyometrial hemabate and pitocin. The total estimated blood loss was 4000 ml and patient received 14 units of packed red blood cells, 9 units of fresh frozen plasma, 2 units of platelets, 750 ml of albumin and 1350 ml of cell saver. During this time, blood pressure was difficult to treat and refractory to multiple vasopressors due to catecholamine withdrawal and alpha blockade. After 10 hours in the operating room, the tumor was successfully excised. Due to significant bowel edema, the abdomen was left open with use of a negative pressure therapy system [6].
The patient remained intubated and required high dose vasopressors until postoperative day 3. Intravenous metoprolol was required to control her tachycardia. On postoperative day 8, she no longer required rate control and she remained normotensive. She returned to the operative room multiple times for abdominal washouts. The newborn was discharged home on day 12 of life. Her fascia was closed on postoperative day 17 and the patient was discharged home 3 days later [7].
Results and Discussion
Paragangliomas, also known as extraadrenal pheochromocytomas are rare catecholamine-secreting tumors. Their occurrence is estimated to be present in one in 54,000 pregnancies. If undiagnosed, maternal mortality is nearly 50%. Early detection and proper management decreases both maternal and fetal mortality to less than 5% and 15% respectively. Management is dependent on the gestational age at the time of PGL diagnosis. When diagnosed before 24 weeks of gestation, the tumor should be excised preferably by a laparoscopic approach in the second trimester. When a paraganglioma is diagnosed in the third trimester, surgical excision should be delayed until after delivery with the tumor excision immediately after delivery or delayed until a later time. Vaginal delivery is associated with increased maternal mortality likely due to sudden release of catecholamines into the circulation due to tumor stimulation and labor contractions; therefore, cesarean delivery should be the mode of delivery (Figure 2) [8].
Prior to surgical management, alpha-receptor blockade is required to control and prevent intraoperative arrhythmia and hypertensive crises. According to the endocrine society, the recommended preoperative medical treatment is 7 to 14 days with phenoxybenzamine, an irreversible alpha-adrenergic antagonist. Phenoxybenzamine is the preferred treatment of choice in women with PPGL7, based on case series, despite no head to head trials to compare it to its counterpart, doxazosin, a competitive alpha-1 selective adrenergic blocker. In this case, our patient received 10 days of alpha blockade with steady titration to phenoxybenzamine 60 mg daily in divided doses with goal systolic blood pressure <140 and heart rate >110. However, due to the rarity of PPGL in pregnancy, target blood pressures, salt intake and fluid intake goals have not been established. In non-pregnancy state, the goal of alpha blockade is to achieve orthostatic hypotension, which is based on nonsystematic observational studies. This goal, however, is challenging in pregnancy as maternal hypotension may lead to a decrease in placental perfusion, therefore our goal was systolic blood pressure was <140 and heart rate <110.
Tumor localization is essential after unequivocal biochemical evidence or suspicion for PPGL. In gravid women, Magnetic Resonance Imaging (MRI) is the gold standard. Paragangliomas can originate at multiple anatomical sites, including the head, neck, thorax and abdomen. Retroperitoneal paragangliomas account for up to 87% of all paragangliomas. This poses a greater challenge in pregnancy, as the gravid uterus is located anterior to the tumor causing undesired tumor stimulation with abdominal palpation, fetal movement and an enlarging uterus with advancing gestational age. In this circumstance, obstetric considerations include avoiding stimulation of the tumor with abdominal palpation and considering cesarean breech extraction or a transfundal incision for breech extraction. Massive hemorrhage from both arterial and venous blood loss should be anticipated especially with retroperitoneal paragangliomas given its position in the aortocaval space. In one retrospective review of 34 resected retroperitoneal paragangliomas at a single institution over a period of 16 years, all tumors exhibited surfaces with a rich blood supply, 13 tumors (38%) were adhered to adjacent tissues and 7 (21%) of the tumors required adjacent organ resection. From an obstetric standpoint, minimization of intraoperative blood loss and DIC may be accomplished with consideration for prophylactic uterine compression sutures in the setting of prolonged surgery, local cytotec use and tranexamic acid administration. In addition, maternal positioning in dorsal lithotomy should be considered prior to cesarean delivery for early recognition of vaginal bleeding and postpartum hemorrhage. In this case, the patient was not placed in dorsal lithotomy as delivery was expedited due to fetal bradycardia after central line placement, which made it challenging to identify vaginal bleeding. A B-lynch compression suture was successfully placed following uterine atony but, in the future, may be considered prophylactically (Figure 3) [9].
Diagnosis of PPGL should prompt a discussion regarding genetic testing for the mother and neonate. Historically, PPGLs were thought to hereditary in only 10% of cases. In recent years, it has been shown that up to one-third of cases are associated with known germline mutations. In this patient’s case, she had multiple family members with reported tumors and hypertension but had not received prior genetic screening. In this case, genetic testing was positive for a germline mutation in the enzyme, Succinate Dehydrogenase that encodes subunit B (SDHB). Mutations in this gene have been reported in families with hereditary Paraganglioma-Pheochromocytoma (PGL/PCC) syndrome, which is inherited in an autosomal dominant manner, giving each child a 50% chance of inheriting the mutation. SDHB mutations are associated with increased risk of malignancy, multiple tumors and recurrences. The endocrine society recommends all patients with PPGLs should engage in shared decision making for genetic testing including the possibility of genetic testing for at-risk relatives of the affected individual. It is important to discuss the inheritance patterns and risk of disease with the mother so that the infant may then be tested and receive appropriate surveillance for early detection [10].
Conclusion
This case demonstrates another preeclampsia mimicry and a rare case of a paraganglioma in a patient diagnosed in the third trimester of pregnancy that was successfully alpha blocked and delivered via cesarean section with tumor excision. The intraoperative challenges highlight the importance of a multidisciplinary approach in a tertiary care center to identify and treat PPGLs as well as anticipate and respond to catastrophic events.
Conflict of Interest
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
References
- Giampaolino P, Della Corte L, Formisano C, Cuomo L, Maurea S, et al. (2018) Successful management of a third-trimester pregnancy complicated by pheochromocytoma: Case report. Gynecol Endocrinol 34: 1016-1018.
[Crossref] [Google Scholar] [PubMed]
- Lenders JW, Langton K, Langenhuijsen JF, Eisenhofer G (2019) Pheochromocytoma and pregnancy. Endocrinol Metabol Clin 48: 605-617.
[Crossref] [Google Scholar] [PubMed]
- Ahlawat SK, Jain S, Kumari S, Varma S, Sharma BK (1999) Pheochromocytoma associated with pregnancy: Case report and review of the literature. Obstet Gynecol Surv 54: 728.
[Crossref] [Google Scholar] [PubMed]
- Wing LA, Conaglen JV, Meyer-Rochow GY, Elston MS (2015) Paraganglioma in pregnancy: A case series and review of the literature. J Clin Endocrinol Metabol100: 3202-3209.
[Crossref] [Google Scholar] [PubMed]
- Schenker JG, Granat M (1982) Phaeochromocytoma and pregnancy-an updated appraisal. J Obstet Gynaecol 22: 1.
[Crossref] [Google Scholar] [PubMed]
- Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, et al. (2014) Pheochromocytoma and paraganglioma: An endocrine society clinical practice guideline. J Clin Endocrinol Metabol 99: 1915-1942.
[Crossref] [Google Scholar] [PubMed]
- Pacak K (2007) Preoperative management of the pheochromocytoma patient. J Clin Endocrinol Metabol 92: 4069-4079.
[Crossref] [Google Scholar] [PubMed]
- Ji XK, Zheng XW, Wu XL, Yu ZP, Shan YF, et al. (2017) Diagnosis and surgical treatment of retroperitoneal paraganglioma: A single-institution experience of 34 cases. Oncol Lett 14: 2268-2280.
[Crossref] [Google Scholar] [PubMed]
- Jaiswal SK, Ya Sarathi V, Memon SS, Goroshi M, Jadhav S, et al. (2019) Sympathetic paraganglioma: A single-center experience from Western India. Endocr Prac 25: 211-219.
[Crossref] [Google Scholar] [PubMed]
- Mayuga KA, Fedorowski A, Ricci F, Gopinathannair R, Dukes JW, et al. (2022) Sinus tachycardia: A multidisciplinary expert focused review. Circulation 15: e007960.
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences