Role of Pelvic Artery Embolisation in Postpartum Hemorrhage
N Navakumar, MK Yadav, R Vidyalekshmy and NA Paul
N Navakumar1*, MK Yadav2, R Vidyalekshmy1 and NA Paul1
1Department of High risk pregnancy and Perinatology, Kerala Institute of Medical sciences, Trivandrum, India
2Department of Interventional Radiology, Kerala Institute of Medical sciences, Trivandrum, India
- Corresponding Author:
- N Navakumar
Department of High risk pregnancy and Perinatology
Kerala Institute of Medical sciences
Trivandrum, India
E-mail: ninanavakumar@yahoo.co.in
Received: March 25, 2021; Accepted: April 13, 2021; Published: April 24, 2021
Citation:Navakumar N, Yadav MK, Vidyalekshmy R, Paul NA (2021) Role of Pelvic Artery Embolisation in Postpartum Hemorrhage. Crit Care Obst Gyne Vol.7 No.3:29.
Abstract
Purpose: To evaluate the safety and efficacy of Pelvic Arterial Embolization (PAE) for the treatment of Primary and secondary Postpartum Hemorrhage (PPH) and to determine the factors associated with clinical outcomes.
Materials and methods: This was a retrospective single-center cohort study in which data was retrieved from electronic medical records. Outcomes were analyzed in 22 patients who underwent PAE for PPH between January 2008-May 2019 over a period of 11 years. Mode of delivery, causes of bleeding, laboratory and treatment records, and clinical outcomes were retrieved. Clinical success was calculated. Univariate analysis was performed to determine the factors related with clinical outcomes.
Results: The mean age of pregnant women included in our study is 28.3 ± 4 years. Most of them had primary PPH-20(90.9 %) patients. 13 (59.1%) patients had coagulopathy. In most of them embolic material used were gel foam and its combination-18 (81.7%). In majority of them uterine artery alone was embolised-12 (54.5%). Only 4.5 % had complications after PAE. The clinical success rate was 17/22 patients (77.3%). Overall mortality was 2 of 22(9%). Univariate analysis showed that Disseminated Intravascular Coagulation (DIC) and massive transfusion of more than 15 red blood cell units were related to failed PAE cases.
Conclusion: PAE is safe and effective for managing primary & secondary PPH. Patients with DIC and massive transfusion were likely to have poor results after pelvic artery embolisation.
Keywords
Postpartum hemorrhage; Metastatic colon cancer; Pelvic artery embolisation; Clinical outcome; DIC; Massive transfusion
Introduction
Postpartum haemorrhage is one of the leading causes of maternal mortality worldwide and may occur immediately or several hours or days after delivery [1,2]. It occurs in 5% of deliveries with a mortality rate of 25% [3,4]. Postpartum haemorrhage is defined as estimated blood loss of 500 ml after vaginal delivery and 1000 ml after caesarean section [5]. Postpartum haemorrhage can be classified as primary and secondary. Primary is when PPH occurs during the first 24 hours after delivery and secondary is when it occurs after 24 hours of delivery [6]. Management of PPH can be medical or surgical, were medical management is reserved for minor PPH (blood loss <1000 ml). Patients with major PPH (blood loss >1000 ml) have conventionally been treated with surgical methods like uterine compression sutures, stepwise devascularisation and hysterectomy [7]. They are associated with increased morbidity and mortality. With recent advances in technology transcatheter embolization has become a very important tool in treating patients with major PPH. The decision to do TAE needs multidisciplinary team approach which includes obstetrician, maternal medicine specialist, intensivist, haematologist, interventional radiologist. The advantages of TAE include easy identification of the bleeding site, preservation of the uterus and fertility. It is also fast, highly effective, minimally invasive with low complication rate, shorter hospital stays and lack need for general anesthesia [8].
Methods
Aim: To evaluate the safety and efficacy of Pelvic Arterial Embolization (PAE) for the treatment of primary and secondary PPH and to determine the factors associated with clinical outcome.
Materials and methods: This was a retrospective single-centre cohort study in which data was retrieved from electronic medical records of KIMS, Trivandrum. Outcomes were analysed in 22 patients who underwent PAE for PPH between January 2008-May 2019 over a period of 11 years.
Patient selection: Who underwent PAE for the treatment of intractable primary and secondary PPH despite medical or obstetric efforts. The potential risks and benefits of PAE were explained to each patient before the procedure; each patient provided written informed consent. A thorough review of the obstetric charts about clinical course, laboratory and treatment records were done to collect the data regarding patient characteristics, cause of bleeding, type of delivery, pre- and postembolization treatments, presence of DIC, the amount of blood transfusion, details of the PAE procedure, complications related to PAE, and the final outcome. Clinical success rate was defined as cessation of bleeding after PAE without the need for surgery and without maternal mortality.
Statistical Analysis: Outcome was compared between successful and failed PAE for selected variables. Univariate analysis was performed to determine the factors related with clinical outcome. Univariate analysis of non-parametric data was assessed by using the Fisher exact test. All statistical analyses were performed by using software (SPSS, version17.0 for Windows; SPSS, Chicago, Ill), and statistical significance was defined as p value less than 0.05.
Results
Our study comprised of 22 patients. The mean age of the patients were 28.3 ± 4 years of which 11 (50%) were nulliparous and 11 (50%) were multiparous. The majority of them 16 (73%) were term deliveries. 6 (27%) patients had a history of previous caesarean section. 13 (59.1%) had vaginal delivery. 20 (90.9%) had primary PPH (Table 1). Most common cause of PPH was atonic PPH 8 (36.4%). 13 (59.1%) of 22 patients had coagulopathy 15 (68.2%) were referred from other hospitals. In majority of the patients gel foam was used alone n=11 (50%) or in combination with other embolic materials (Table 2). 12 (54.5%) patients were in hemorrhagic shock at the time of embolization. Bilateral uterine artery embolization 9 (40.9%) was the commonest procedure done (Table 3). Pre procedure 14 (63.6%) patients had severe anaemia (<7g/dl of Hb) whereas post procedure 19 (86.4%) patients hemoglobin was more than or equal to >7 g/dl. 11 (50%) of patients needed ventilatory support. 15 (68.2%) had comorbid conditions. 4 (18.2%) patients underwent uterine compression sutures or stepwise devascularization. 3 (13.6%) who underwent hysterectomy for PPH required further PAE after surgical intervention for ongoing bleeding. 17 (77.3%) cases had positive findings in CT angiogram in our study. Most common significant CT angiogram observations was extravasation of contrast in 9 (40.9%) (Table 4). Extravasation of contrast was associated with DIC in majority of cases.
| PPH | Frequency | Percentage |
|---|---|---|
| Atomic | 8 | 36.4 |
| Traumatic | 3 | 13.6 |
| DIC | 1 | 4.5 |
| Adherent placenta | 1 | 4.5 |
| Retained placenta | 1 | 4.5 |
| Pseudo aneurysm | 2 | 9.1 |
| Sepsis | 3 | 13.6 |
| Multifactorial | 3 | 13.6 |
| Total | 22 | 100 |
Table 1: Causes of PPH.
| Embolic Material | Frequency | Percentage |
|---|---|---|
| Gelfoam | 11 | 50 |
| NCBA | 2 | 9.1 |
| PVA+Gelfoam | 5 | 22.7 |
| NCBA+Gelfoam | 1 | 4.5 |
| NCBA+PVA+Gelfoam | 1 | 4.5 |
| PVA+Coil | 1 | 4.5 |
Table 2: Embolic agent used.
| Artery | Frequency | Percentage |
|---|---|---|
| Unilateral Uterine Artery | 3 | 13.6 |
| Bilateral Uterine Artery | 9 | 40.9 |
| Vaginal Artery | 3 | 13.6 |
| Bilateral Uterine+Inferior Epigastric+Obturator Artery | 2 | 9.1 |
| Bilateral Internal iliac Artery | 4 | 18.2 |
| Bilateral Internal iliac + Uterine Artery | 1 | 4.5 |
Table 3: Artery embolised.
| Angiogram observations | Frequency | Percentage |
|---|---|---|
| No dye extravasation | 5 | 22.7 |
| Dye extravasation | 9 | 40.9 |
| Pseudoaneurysm | 2 | 9.1 |
| Hypertrophy | 5 | 22.7 |
| Spasm | 1 | 4.5 |
| Total | 22 | 100 |
Table 4: Angiogram observation.
Of the 22 patients who underwent PAE, bleeding was successfully controlled in 17 patients. The clinical success rate was 77.3%. In 5 patients, PAE failed to control hemorrhage and 4 out of the 5 patients had to undergo hysterectomy. 2 (9.09%) out of 22 patients died. Fever was the only procedure related complication which was seen in 1 (4.5%). Univariate analysis of the data showed statistical significance for DIC (p=0.034) and massive blood transfusion (p=0.001) more than 15 units of blood products as predictors of failure for PAE in PPH (Table 5).
| Failure | |||||||
|---|---|---|---|---|---|---|---|
| No | Yes | Total | |||||
| Variable | N | % | N | % | N | % | p value |
| I PPH |
- | - | - | - | - | - | |
| 0.421 | |||||||
| Primary PPH | 15 | 88.2 | 5 | 100 | 20 | 90 | |
| Secondary PPH | 2 | 11.8 | 0 | 0 | 2 | 9.1 | |
| Cause of PPH | |||||||
| Atonic | 6 | 35.3 | 2 | 40 | 8 | 36.4 | |
| DIC | 3 | 17.6 | 1 | 20 | 4 | 18.2 | 0.962 |
| Others | 8 | 47.1 | 2 | 40 | 10 | 45.5 | |
| DIC | |||||||
| No | 9 | 52.9 | 0 | 0 | 9 | 40.9 | |
| Yes | 8 | 47.1 | 5 | 100 | 13 | 59.1 | 0.034* |
| Embolic Material | |||||||
| Gelfoam | 8 | 47.1 | 3 | 60 | 11 | 50 | |
| PVA+gelfoam | 4 | 23.5 | 1 | 20 | 5 | 22.7 | 0.871 |
| Combination | 5 | 29.4 | 1 | 20 | 6 | 27.3 | |
| Shock | |||||||
| No | 9 | 52.9 | 1 | 20 | 10 | 45.5 | |
| Yes | 8 | 47.1 | 4 | 80 | 12 | 54.5 | 0.193 |
| Time from delivery | |||||||
| =1 day | 10 | 58.8 | 4 | 80 | 14 | 63.6 | |
| =2 days | 7 | 41.2 | 1 | 20 | 8 | 36.4 | 0.387 |
| Blood transfusion | |||||||
| <15 | 15 | 93.8 | 1 | 20 | 16 | 76.2 | |
| >15 | 1 | 6.2 | 4 | 80 | 5 | 23.8 | 0.001* |
| CT Observation | |||||||
| No dye extravasation | 3 | 17.6 | 2 | 40 | 5 | 22.7 | |
| Dye extravasation | 14 | 82.4 | 3 | 60 | 17 | 77.3 | 0.294 |
| Co-morbidity | |||||||
| No | 7 | 41.2 | 0 | 0 | 7 | 31.8 | |
| Yes | 10 | 58.8 | 5 | 100 | 15 | 68.2 | 0.082 |
Table 5: Univariate analysis.
Discussion
Postpartum haemorrhage is the leading cause of maternal death in low-income countries and a quarter of deaths worldwide [9]. Surgical treatment is required when conservative management fails to manage PPH but it is associated with significant morbidity and mortality. In 1979 Brown et al. reported trans catheter embolization for internal illac arteriesor uterine arteries to control PPH [10]. Since then, trans catheter embolization has come along in a big way and is the preferred option in centers were it is available round the clock [11].
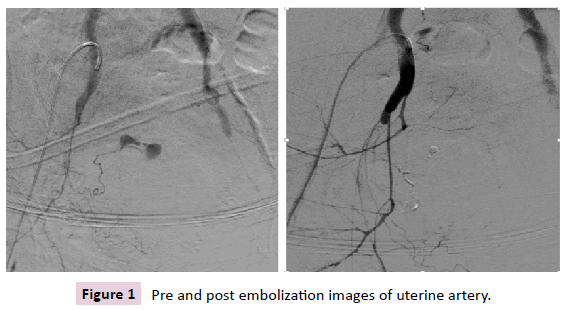
Most common cause for PPH in our study was uterine atony which was also the common cause in studies by Miyuki et al. [12]. The other common indications for TAE were traumatic PPH, retained placenta and infections which were similar to findings of Chen et al. [13]. CT angiogram was used whenever bleeding was suspected from vessels other than uterine arteries and contrast extravasation was the commonest finding in 9 (40.9%) patients out of 22 which was comparable to a study by Miyuki et al. [12]. Active extravasation of contrast medium in angiography are considered as active bleeding points but negative findings on angiography do not exclude bleeding (Figure 1). The failure rate was more if angiogram showed extravasation [13].
In our study the clinical success rate was 77.3% compared to a meta-analysis by Sathe et al which demonstrated clinical success rates of PAE ranging from 58% to 98% with median success rate of 89% [14,15]. In our study it was seen that success rate of PAE for secondary PPH was 100% whereas for primary was 75%. Clinical success involves many factors such as time lapse between onset of PPH and intervention, prompt diagnosis, early intervention, 24 hours availability of trained professionals and infra-structure for PAE, timely management of coagulopathy and blood bank facilities. In other studies it was seen that factors more frequently causing failed embolization were DIC, haemodynamic instability, haemoglobin less than 8g/dl, massive blood transfusion and extravasation [13]. Detected on angiography and however in our study only DIC and massive blood transfusion showed statistical significant correlation as predictors for failed PAE [16]. Most of the cases in our study were referred cases with delay in transfers who had coagulopathy and haemodynamic instability which could account for the decreased clinical success compared to other studies. Though presence of DIC showed statistical significant correlation with failure rate still PAE may be the only option in haemodynamically unstable patients, with multiorgan failure and for patients on ventilatory support. To improve clinical success of embolisation in DIC, early intervention is recommended.
In previous studies the complication rates after PAE were ranging between 3%-9% in our study it was 4.5% which was attributed to post procedure fever in a single patient [17]. The major and minor complications of PAE described are post embolization syndrome, vascular perforation, lower limb ischemia, haematoma at puncture site, pelvic infection and uterine necrosis, however in our study we did not come across any major complications of PAE.
The most common embolic material used in our patients was gel foam (temporary agent) and its combinations which was similar to studies by Soyer et al. and Dohan et al. [18,19] N Butyl Cyanoacrylate (NBCA) was used for traumatic PPH. NBCA alone or as combination with other embolic agents were used in 4 (18.2%) patients in our study. In a study by Park et al. results showed that use of NBCA had better success rates in pseudoaneurysm and extravasation [20].
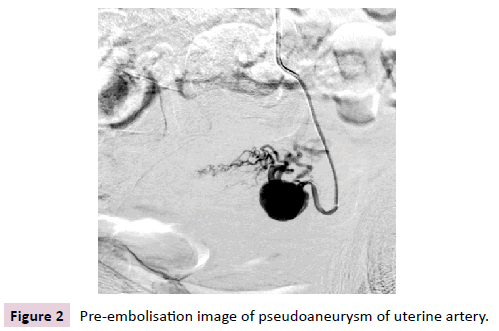
Uterine arteries were the commonest arteries embolised [21]. Uterine arteries alone were embolised in 54.5% of cases in our study. Uterine arteries and internal iliac arteries were selected when there was no evidence of extravasation in CT angiogram while super selective embolization of other pelvic arteries were done in the presence of extravasation in cases of traumatic PPH and pseudoaneurysm (Figure 2).These findings were comparable with previous study by Sone et al. [12].
The advantage of performing PAE over surgical interventions such as hysterectomy is in achieving haemostasis without sacrificing the reproductive ability of the patient [17]. As step wise devascularisation in PPH may fail to stop bleeding due to collateral circulation and emergency hysterectomy is associated with high morbidity and mortality PAE is preferred in selected cases [22]. In our study PAE after caesarean hysterectomy was done in 3 (13.6%) and was done along with compression sutures/ step wise devascularisation in 4 (18.2%) to control bleeding. In a study by Lee MJ et al. it was concluded that PAE for persistent PPH after hysterectomy is a safe and effective treatment. The other advantages are easy identification of bleeding site, decreased rebleeding from collaterals with more distal occlusion of bleeding vessels. The earlier PAE is done less the blood loss and easier subsequent surgery with a clear field of vision. Resumption of regular menstrual cycle was demonstrated in 97.3% of 251 patients with reporting of subsequent pregnancies [17].
The mortality rate after PAE including that after surgery is <2%. Mortality directly attributable to PAE have not been reported [12]. In our study mortality rate was 2 (9%), both were late hospital transfers with multiorgan failure, DIC and shock.
Our first case with mortality was a 34-year-old second gravid, referred for dengue complicating pregnancy had preterm vaginal delivery, went into shock and coagulopathy with dengue hepatitis. She developed primary atonic PPH for which CT angiogram was done which showed severe spasm of internal iliac vessels. Embolization was performed with PVA and gel foam on postnatal day 1. But patient had persistent bleeding and refractory DIC. She underwent hysterectomy and relaparotomy with bilateral internal iliac artery ligation. She was ventilated and received massive blood transfusion, diagnosed with severe refractory dengue shock syndrome but patient succumbed on day 11.
Our second case was a 28-year-old primigravida at term referred with intra-uterine fetal demise with acute fatty liver of pregnancy, sepsis, and multiorgan failure. Stillborn was delivered by caesarean section, developed primary PPH and refractory coagulopathy which did not improve with massive blood transfusions. CT angiogram showed no extravasation of pelvic arteries hence nonselective bilateral internal iliac artery embolisation with gelfoam was performed however post embolisation patient had persistent bleeding, and succumbed on day 5.
Conclusion
PAE is safe and effective for managing primary and secondary PPH. Patients with DIC and massive transfusion were likely to have unfavourable outcomes after pelvic artery embolisation. PAE can be considered as the standard second line option to treat PPH and first-line therapy in patients who are refractory to conservative measures. A rapid transfer is critical for persistent bleeding after delivery to save maternal lives. The availability of a multidisciplinary team, including the use of pelvic artery embolization, was vital in averting maternal mortality despite significant morbidity with preservation of fertility.
Limitations
• The first limitation of our study was its retrospective design
• The second limitation was that the sample size is too small
• The third limitation the time interval between onset of PPH and PAE intervention could not be assessed as many of them were referred cases
• The fourth limitation of our study was lack of control group
Acknowledgments
I acknowledge contribution of my co-authors, my institution and all those who helped me to complete this study.
Funding/Conflicts of Interests
We report no funding assistance or conflicts of interest.
References
- Yalinkaya A, Güzel AI, Kangal K (2010) Emergency Peripartum Hysterectomy 16-year experience of a medical hospital. J Chin Med Assoc 73: 360-363
- Yang MJ, Wang PH (2010) Peripartum hysterectomy risk factors in Taiwan. J Chin Med Assoc 73: 399-400.
- Reitman E, Devine PC, Laifer-Narin SL, Flood P (2011) Case scenario: perioperative management of a multigravida at 34-week gestation diagnosed with abnormal placentation. J Ame Soc of Anaesth 115: 852-857.
- Rossi AC, Mullin P (2012) The etiology of maternal mortality in developed countries: a systematic review of literature. Arch Obstet Gynaecol 285: 1499-1503.
- Stafford I, Dildy GA, Clark SL, Belfort MA (2008) Visually estimated and calculated blood loss in vaginal and cesarean delivery. Ame J of Obstet Gynaecol 199: 519-e1.
- Delotte J, Novellas S, Koh C, Bongain A, Chevallier P (2009) Obstetrical prognosis and pregnancy outcome following pelvic arterial embolisation for post-partum hemorrhage. Eur J Obstet Gynecol Reprod Biol 145: 129-132.
- No GG (2016) Prevention and management of postpartum haemorrhage. BJOG. 2016124: e106-49.
- Wee L, Barron J, Toye R (2004) Management of severe postpartum haemorrhage by uterine artery embolization. Br J Anaesth 93: 591-594.
- Say L, Chou D, Gemmill A, Tunçalp O, Moller AB, et al. (2014) Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health 2: 323-333.
- Brown BJ, Heaston DK, Poulson AM, Gabert HA, Mineau DE, et al. (1979) Uncontrollable postpartum bleeding: a new approach to hemostasis through angiographic arterial embolization. Obstet Gynaecol 54: 361-365.
- Morel O, Malartic C, Muhlstein J, Gayat E, Judlin P, et al. (2011) Pelvic arterial ligations for severe post-partum hemorrhage. Indications and techniques. J Visc Surg 148: 95-102.
- Sone M, Nakajima Y, Woodhams R, Shioyama Y, Tsurusaki M, et al. (2015) Interventional radiology for critical hemorrhage in obstetrics: Japanese Society of Interventional Radiology (JSIR) procedural guidelines Jpn J Radiol 33: 233-240.
- Chen C, Lee SM, Kim JW, Shin JH (2018) Recent update of embolization of postpartum hemorrhage. Korean J Radiol 19: 585.
- Yang IP, Miao ZF, Huang CW, Tsai HL, Yeh YS, et al. (2019) High blood sugar levels but not diabetes mellitus significantly enhance oxaliplatinchemoresistance in patients with stage III colorectal cancer receiving FOLFOX6 chemotherapy. Ther Adv Med Oncol 11: 1-13.
- Touboul C, Badiou W, Saada J, Pelage JP, Payen D, et al. (2008) Efficacy of selective arterial embolisation for the treatment of life-threatening post-partum haemorrhage in a large population. PLoS One, 3: 3819.
- Kim YJ, Yoon CJ, Seong NJ, Kang SG, Kim YS, et al. (2013) Failed pelvic arterial embolization for postpartum hemorrhage: clinical outcomes and predictive factors. J Vasc Interv Radiol 24: 703-709.
- Lee HY, Shin JH, Kim J, Yoon HK, Ko GY, et al. (2012) Primary postpartum hemorrhage: outcome of pelvic arterial embolization in 251 patients at a single institution. Radiol 264: 903-909.
- Soyer P, Dohan A, Dautry R, Guerrache Y, Ricbourg A, et al. (2015) Transcatheter arterial embolization for postpartum hemorrhage: indications, technique, results, and complications. J Vasc Interv Radiol, 38: 1068-1081.
- Dohan A, Pelage JP, Soyer P (2013) How to avoid uterine necrosis after arterial embolization for post-partum hemorrhage: a proposal based on a single center experience of 600 cases. Eur J Obstet Gynecol Reprod Biol, 171: 392-393.
- Park KJ, Shin JH, Yoon HK, Gwon DI, Ko GY et al. (2015) Postpartum hemorrhage from extravasation or pseudoaneurysm: efficacy of transcatheter arterial embolization using N-butyl cyanoacrylate and comparison with gelatin sponge particle. J Vasc Interv Radiol, 26: 154-161.
- Labarta FR, Recarte MP, Luque AA, Prieto LJ, Martín LP, et al. (2016) Outcomes of pelvic arterial embolization in the management of postpartum haemorrhage: a case series study and systematic review. Eur J Obstet Gynecol Reprod Biol 206: 12-21.
- Gizzo S, Saccardi C, Patrelli TS, Di Gangi S, Breda E, et al. (2013) Fertility rate and subsequent pregnancy outcomes after conservative surgical techniques in postpartum hemorrhage: 15 years of literature. F S Rep 99: 2097-2107.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences