Medical Treatment of Interstitial (Cornual) Ectopic Pregnancy with Methotrexate: A Case Report
Moeeneh Barkhori Mehni1*, Mahdi Barkhori Mehni2
Moeeneh Barkhori Mehni1*, Mahdi Barkhori Mehni2
1Department of Obstetrics and Gynecology, School of Medicine, Jiroft University of Medical Sciences, Jiroft, Iran
2Department of Obstetrics and Gynecology , Tehran University of Medical Sciences, Tehran, Iran
- *Corresponding Author:
- Moeeneh Barkhori Mehni
Department of Obstetrics and Gynecology
School of Medicine
Jiroft University of Medical Sciences
Jiroft
Iran
Tel: +98 34 43319085
E-mail: hshafieemojaz65@gmail.com
Received Date: May 13, 2021; Accepted Date: September 06, 2021; Published Date: September 16, 2021
Citation: Moeeneh B M (2021) Medical Treatment of Interstitial (Cornual) Ectopic Pregnancy with Methotrexate: A Case Report. Crit Care Obst Gyne Vol. 07 No. 04.
Abstract
Ectopic pregnancy (EP) is a pregnancy outside of uterus and accounts for 1-4% of all pregnancies. The most common risk factors for EP include the use of assisted reproductive techniques and tubular and uterine abnormalities (history of surgery or previous ectopic pregnancy, leiomyoma, endometriosis, history of pelvic infection, etc.). One type of tubal ectopic pregnancy is the interstitial (cornual) type, which is responsible for 1-6% of ectopic pregnancies and 20 % of all deaths caused by them.
Abstract
Ectopic pregnancy (EP) is a pregnancy outside of uterus and accounts for 1-4% of all pregnancies. The most common risk factors for EP include the use of assisted reproductive techniques and tubular and uterine abnormalities (history of surgery or previous ectopic pregnancy, leiomyoma, endometriosis, history of pelvic infection, etc.). One type of tubal ectopic pregnancy is the interstitial (cornual) type, which is responsible for 1-6% of ectopic pregnancies and 20 % of all deaths caused by them.
Although the main treatment for ectopic pregnancy is still surgery, due to advances in rapid diagnosis, many women today are taking medical treatment with Methotrexate (MTX) as treatment for ectopic pregnancy. Due to the high risk of bleeding, many physicians prefer to use surgical methods (hysterectomy or cornual wedge resection) for the treatment of interstitial ectopic pregnancy. In this article we discuss a woman with an interstitial ectopic pregnancy who responded to methotrexate treatment and was discharged from the hospital in a stable general condition.
Keywords
Ectopic pregnancy, Interstitial ectopic pregnancy, Cornual ectopic pregnancy, Medical management, Methotrexate
Introduction
EP is a pregnancy outside of uterus that accounts for 1-4% of all pregnancies[1]. EP occurs mainly in the fallopian tube (84%) [2, 3]. The most common risk factors for EP include the use of assisted reproductive techniques and tubular and uterine abnormalities (history of surgery or previous EP, leiomyoma, endometriosis, history of pelvic infection, etc.) [4].
Interstitial EP is a rare type of EP in which implantation occurs in the earliest part of the fallopian tube that passes through the myometrium. The interstitial type is responsible for 1-6% of all EPs but 20 % of all deaths caused by EPs[5, 6] and its incidence has been increasing in the last two decades due to the use of assisted reproductive techniques[7]. Maternal mortality rate of interstitial EP (2.0-2.5%) is higher than other forms of EP due to delayed diagnosis and high vascularity of the myometrium[6, 8].
Due to the high risk of bleeding, many physicians prefer to use surgical methods (hysterectomy or cornual wedge resection) for the treatment of interstitial EP despite its high morbidity and impact on future fertility[9, 10].
Although the main treatment for EP is still surgery, due to advances in rapid diagnosis, many women today are taking medical treatment with MTX as treatment for EP [4, 11, 12] although MTX treatment is more effective in cases where early diagnosis is made[9].
Today, with the advancement of technology, it is possible to radiologically and biochemically diagnose EP at an earlier stage, and this can help the use of non-invasive medical treatment in EP.
Since 1982, when MTX was first used to treat EP [13], no consensus has been reached on interstitial EP treatment method.
In this article we talk about a 30-year-old pregnant woman (G4, P3) with interstitial EP, gestational age of 5 weeks and 3 days and βHCG level of 9187 mIU/mL at first day of admission, who was successfully treated with 4 doses of systemic MTX each 1 mg/kg.
Case Report
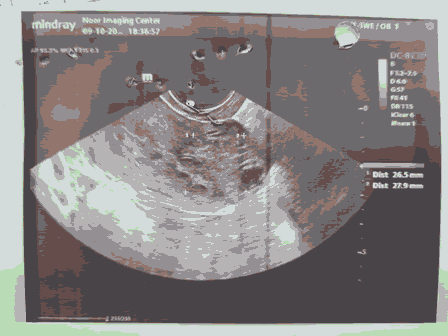
A 30-year-old opium addicted woman weighing 40 kg, with her fourth pregnancy and three healthy children born by natural vaginal delivery (G4, P3), referred to our center with complaint of vaginal bleeding. The patient was diagnosed with interstitial EP in ultrasound as shown in Figure 1.
According to the last menstrual period (LMP), the patient's gestational age at the day of first visit was 5 weeks and 3 days. In the performed transvaginal sonography (TVS), interstitial EP was mentioned as a probable cause of vaginal bleeding. According to this finding, level of βHCG was measured to rule out interstitial EP, which was 9187 mIU/ml. Requested tests included complete blood count (CBC), blood group, haemoglobin, Blood urea nitrogen (BUN), Creatinine (Cr), total and direct bilirubin. On the first day of hospitalization, the hemoglobin level was 10 gr/dl and other tests were in normal range. The results of the laboratory tests performed during the patient's hospital stay are shown in Table 1.
| Day 1 | Day 3 | Day 5 | Day 7 | |
|---|---|---|---|---|
| WBC | 8000 | 4700 | 5400 | 6000 |
| RBC | 4.36 | 4.16 | 4.74 | 4.78 |
| Hemoglobin | 10 | 9.4 | 11.1 | 11.6 |
| Hematocrit | 30.7 | 29.2 | 33.5 | 33.6 |
| MCV | 70.4 | 70.2 | 70.7 | 70.3 |
| MCH | 22.9 | 22.6 | 23.4 | 24.3 |
| MCHC | 32.6 | 32.2 | 33.1 | 34.5 |
| Platelets | 204 | 158 | 198 | 192 |
| Urea | 27.2 | 22.1 | 18 | 23 |
| Creatinine | 1.07 | 0.79 | 0.81 | 0.85 |
| S.G.O.T (AST) | 22 | 21 | 22 | 26 |
| S.G.P.T (ALT) | 18 | 15 | 18 | 26 |
| Bilirubin Total | 0.23 | 0.42 | 0.4 | 0.35 |
| Bilirubin Direct | 0.09 | 0.15 | 0.12 | 0.14 |
| LDH | 236 | 253 |
The patient was admitted with βHCG= 9187 mIU/ml and due to the patient's stable general condition, MTX with dose of 1mg/kg was started for her. One day after each dose of MTX, also 4 mg of folinic acid (leucovorin) was administered to the patient.
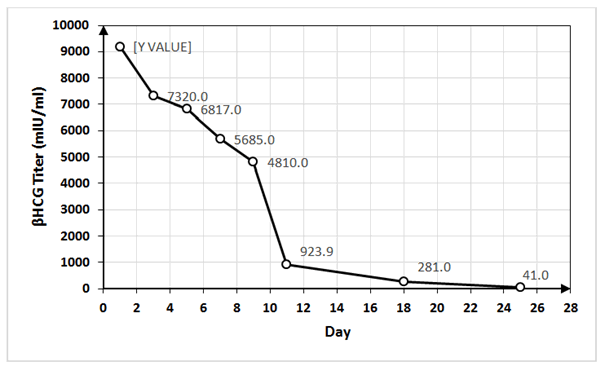
On the first, third, fifth and seventh days of hospitalization, the patient was prescribed with MTX at a dose of 1 mg/kg. The βHCG titer measured on the first, third, fifth, seventh, ninth and eleventh days was 9187, 7320, 6817, 5685, 4810 and 923.9 mIU/ml, respectively. After receiving the fourth dose of MTX, we measured the patient's βHCG level every 48 hours. In consecutive measurements, βHCG level was declining and finally the patient was discharged from the hospital with βHCG titer of 923.9 mIU/ml. During the hospital stay, the patient's laboratory tests were normal.
During treatment, we checked the patient for vital signs, abdominal pain, and MTX complications such as stomatitis, diarrhea, and bone marrow suppression, which ultimately, we didn’t notice any complications. After discharge, we checked the patient's βHCG level weekly. In the first measurement after discharge, the βHCG titer was 281 mIU/ml and in second one was 41 mIU/ml. The related data about MTX and folinic acid dose administered and βHCG titer are shown in Table 2 and Figure 2.
| Day | MTX dose | folinic acid dose | ßHCG titer in mIU/ml |
|---|---|---|---|
| 1 | 40 mg | 9187 | |
| 2 | 4 mg | ||
| 3 | 40 mg | 7320 | |
| 4 | 4 mg | ||
| 5 | 40 mg | 6817 | |
| 6 | 4 mg | ||
| 7 | 40 mg | 5685 | |
| 8 | 4 mg | ||
| 9 | 4810 | ||
| 11 | 923.9 | ||
| 18 | 281 | ||
| 25 | 41 |
Table 2: MTX and folinic acid dose administered and βHCG titer.
Discussion
Interstitial EP is a rare form of EP and is responsible for only1-6% of them[6] and therefore not much information is available about its different treatment options. At present, surgical treatment is the main method of treatment, but with advances in diagnostic methods and diagnosis being made in earlier stages, as shown in our case and several other cases such as Galani, A et al.[14], medical therapy with MTX can be considered in patients with stable general condition and hemodynamics as a reasonable treatment option. In medical treatment with MTX, the patient should be monitored for βHCG level and side effects of the drug, as rupture of the uterus or fallopian tube and MTX side effects can lead to maternal morbidity and even mortality.
Further studies are needed to answer a variety of questions, including which patients can receive MTX medication and which will require surgery.
References
- Park JE (2018) Ectopic pregnancy incidence in the Republic of Korea in 2009–2015: A population-based cross-sectional study. Scientific reports 8(1): 1-5.
- Bouyer J (2002) Sites of ectopic pregnancy: a 10 year population-based study of 1800 cases. Human reproduction 17(12): 3224-3230.
- Rana P (2013) Ectopic pregnancy: a review. Archives of gynecology and obstetrics 288(4): 747-757.
- Yassin AS, MS Taha (2017) Interstitial ectopic pregnancy, Diagnosis and management: a case report and literature review. Ann Clin Case Rep 2(2017): 1352.
- Parker VL, M Srinivas (2016) Non-tubal ectopic pregnancy. Archives of gynecology and obstetrics 294(1): 19-27.
- Stabile G (2020) Conservative Treatment of Interstitial Ectopic Pregnancy with the Combination of Mifepristone and Methotrexate: Our Experience and Review of the Literature. BioMed research international; 2020.
- Rastogi R (2008) Interstitial ectopic pregnancy: A rare and difficult clinicosonographic diagnosis. Journal of human reproductive sciences 1(2): 81.
- Moawad NS (2010) Current diagnosis and treatment of interstitial pregnancy. American journal of obstetrics and gynecology 202(1): 15-29.
- Liao CY (2017) Cornual wedge resection for interstitial pregnancy and postoperative outcome. Australian and New Zealand Journal of Obstetrics and Gynaecology 57(3): 342-345.
- Fisch J (1998) Medical management of interstitial ectopic pregnancy: a case report and literature review. Human reproduction (Oxford, England) 13(7): 1981-1986.
- Lau S, T Tulandi (1999) Conservative medical and surgical management of interstitial ectopic pregnancy. Fertility and sterility 72(2): 207-215.
- Tanaka T (1982) Treatment of interstitial ectopic pregnancy with methotrexate: report of a successful case.
- Galani A (2021) Successful conservative medical management of an interstitial ectopic pregnancy at 10 weeks of gestation: A case report. Case Reports in Women's Health 29: e00284.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences