Laparoscopic Management of Bilateral Ovarian Torsion Following Ovarian Hyperstimulation Syndrome in a Twin Pregnancy
Flavio Grauso, Giuseppe Rosario Lannino and Ciro Perone
DOI10.21767/2471-9803.1000157
Advanced Endoscopic Gynaecological Surgery Center, Sanatrix Clinic, Naples, Italy
- *Corresponding Author:
- Flavio Grauso
Advanced Endoscopic Gynaecological Surgery Center
Sanatrix Clinic – San Domenico, 31, 80127 – Naples, Italy
Tel: +39 3385290037
Fax: +39 081 7173500
E-mail: flaviograuso@gmail.com
Received date: April 15, 2018; Accepted date: April 20, 2018; Published date: April 27, 2018
Citation: Grauso F, Lannino RG, Perone C (2018) Laparoscopic management of bilateral ovarian torsion following ovarian hyperstimulation syndrome in a twin pregnancy. Crit Care Obst Gyne. Vol.4 No.2:4. doi: 10.21767/2471-9803.1000157
Copyright: © 2018 Grauso F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Ovarian accidents requiring surgical intervention during pregnancy should be accurately evaluated to identify the patients who need prompt surgical interventions from those where a “wait-and-see” strategy can be followed. The benefits and safety of minimally invasive surgery are well known in non-pregnant patients, but during pregnancy the risks of laparoscopic approach seems to increase. This is the first case reported in the international literature with bilateral ovarian torsion following ovarian hyperstimulation syndrome in a twin pregnancy, which was successfully managed by laparoscopic ovarian detorsion and unilateral adnexectomy. Increasing evidence suggests that laparoscopic treatment of adnexal masses in pregnancy is safe and effective although it is a surgical challenge with difficulty level that increases with gestational age. For this reason, laparoscopic surgery during pregnancy should be reserved for experienced surgeons able to reduce the additional risks and operating time.
Keywords
Bilateral ovarian torsion; Laparoscopic detorsion; Ovarian hyperstimulation syndrome; Twin pregnancy
Introduction
The benefits and safety of minimally invasive surgery are well known in non-pregnant patients, but during pregnancy an enlarged uterus with a vulnerable embryo-fetus, increases the risk of injury with the Veress needle or trocars. Moreover, fetal acidosis, maternal venous stasis and deep vein thrombosis, associated with the CO2 pneumoperitoneum, can affect maternal fetal health [1,2]. Due to these potential adverse effects, laparoscopic surgery during pregnancy had been considered inappropriate, but its safety and use have become accepted [1]. Up to 1 in 500 to 1 in 635 pregnant women may present a pathology requiring non-obstetric surgery during their pregnancy [3]. Ovarian torsion is rare during gestation, developing in only one in 5000 pregnancies [4]. Most ovarian torsion in pregnancy occurs in the first trimester and it should be suspected for all acute abdominal pain because early diagnosis and intervention lead to a better outcome for the mother and fetus [5]. Ovarian Hyperstimulation Syndrome (OHSS) is characterized by formation of multiple cysts and the enlargement of the ovaries. OHSS primarily occurs in the context of infertility treatments increasing the risk of ovarian torsion (12-25% of pregnant women) [6]. A review of international literature suggests that this is the first case reported with bilateral ovarian torsion following ovarian hyperstimulation syndrome in a twin pregnancy, which was successfully managed by laparoscopic ovarian detorsion and unilateral adnexectomy.
Case Report
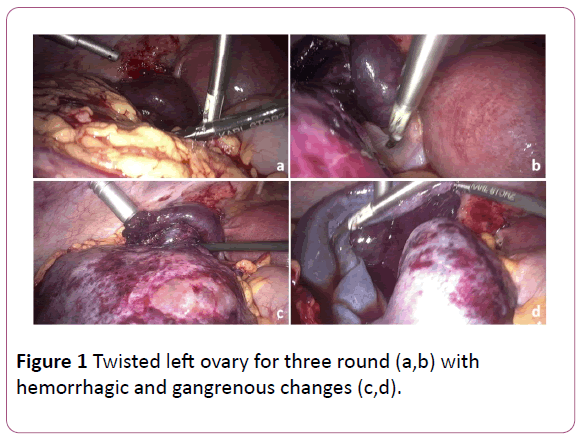
A 33-year-old woman, gravida 2, para 1, was admitted to our center at 10 weeks’ gestation for severe abdominal pain of three weeks duration. She was suspected to have ovarian hyperstimulation syndrome after induction of ovulation with clomid and human menopausal gonadotropins. She had no relevant medical or surgical history. Physical examination showed mild abdominal tenderness and severe lower abdominal pain. Ultrasonography showed normal dichorionic-diamniotic gestation and enlarged ovaries with absent blood flow in the bilateral ovaries. There was a conspicuous fluid accumulated in the cul-de-sac. Laboratory data showed: haemoglobin 6.7 g/dL, haematocrit 21%, white blood cell count 12,730/mL, and platelets 148,000/mL. Biochemistry and thyroid function were normal. An experienced laparoscopic surgeon (C.P.) performed the surgery in about 30 minutes. Laparoscopy confirmed bilateral ovarian torsion and hemoperitoneum, after the lysis of adhesions presumably due to the inflammatory process. The left ovary (measuring 10 cm in maximum diameter) was seen to be twisted for three rounds with haemorrhagic and gangrenous changes (Figure 1), so right left salpingo-oophorectomy was performed.
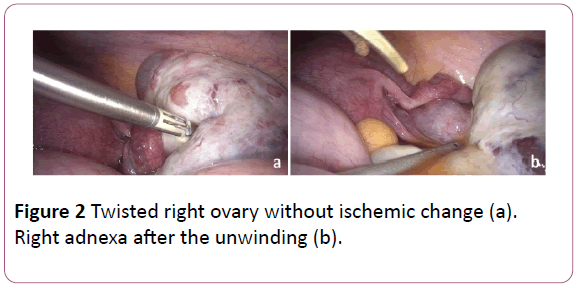
The right ovary (measuring 8 cm in maximum diameter) was also twisted but without ischemic change (Figure 2), so detorsing of the right adnexa was done. The postoperative period was uneventful, and the patient was discharged on the third day. The histologic examination confirmed a necrotic ovary. The laparoscopic surgery was performed according to the current guideline [7,8] following specific recommendations [4]: the patients was placed in a supine position with a 15° left lateral tilt in order to avoid a possible decrease in venous return to the heart; pneumoperitoneum was performed through the Palmer Point with a Verres insufflation needle and was maintained at 14 mmHg; an 11 mm 3D optical laparoscope was introduced through a supraumbilical trocar; under direct visualization three other accessorial trocars were positioned ensuring the efficacy of the intervention without uterine manipulation; haemostasis was achieved by the mild application of bipolar energy. Before and after surgery, ultrasound evaluation showed a normal heart rate in both foetuses. Antepartum monitoring was scheduled every two weeks: 120 days follow-up showed a twin pregnancy in evolution. An informed consent was signed by patient related to use and publication of data, information and any accompanying images.
Discussion
Ovarian accidents, such as torsion and rupture, which complicate OHSS are known but rare events in pregnancy. Ovarian enlargements during pregnancy should be accurately evaluated to identify the patients who need surgical interventions from those where a “wait-and-see” strategy can be followed. Our case highlights the importance of a prompt diagnosis in all pregnant patients presenting with signs and symptoms of acute abdomen and ovarian masses, because OHSS can be associated with life-threatening complications that require early diagnosis for successful management. In our case, indeed the conservative treatment was only possible on the right side, because gangrenous changes of the left ovary required adnexectomy. The assessment of the extent of ovarian ischemia is the greatest difficulty in deciding the surgical management, which is either untwisting for ischemic adnexa or adnexectomy if gangrene has developed [9]. The macroscopic ischemic-hemorrhagic appearance of the affected ovary simulating gangrene could be attributed to venous and lymphatic stasis. On performing detorsion of the ovaries, a significant colour change must be assessed because this implies impeded blood supply, but not complete cessation of the same. In this case a conservative treatment should be preferred [10]. Oelsner et al. which involved a retrospective analysis of 102 patients managed with surgical interventions for adnexal torsion, reported that 91.3% of patients with bluish-black ovary regained normal function. None of the patients developed pelvic or systemic thrombo-embolism, the risk presumed to occur following detorsion of the adnexa [10]. Today, there is widespread debate about open versus laparoscopic approach in non-obstetric surgery during pregnancy. In a large series, there were no differences between open versus laparoscopic approach in perinatal outcomes [11]. However, in a systematic review and meta-analysis by Wilasrusmee comparing laparoscopic and open appendicectomy in pregnancy, the group undergoing laparoscopy showed a greater risk of foetal loss, with no significant differences in preterm delivery, birth weight, Apgar score or wound infection after surgery [12]. These results are consistent with those described in the review by Walsh et al. that showed a significantly higher rate of foetal loss in the laparoscopy group [13]. Nonetheless, the data currently available from retrospective study or individual case report are limited to demonstrate the benefits of one procedure over another. Increasing evidence suggests that laparoscopic treatment of adnexal masses in pregnancy is safe and effective [4,7,14]. Nevertheless, it is surgical challenge with difficulty level that increases with gestational age [4]; indeed, pregnancy increases some risks of the procedure: the enlarged uterus and the lack of uterine manipulator may hinder vision of the surgical field and may also make difficult the port placement or the instauration of pneumoperitoneum; the foetus may be compromised by the alteration in maternal haemodynamic caused by the patient position and intra-abdominal pressure; the foetal acid-base imbalance may be altered by CO2 penumoperitoneum [4]. Historical recommendations were thought to minimize the spontaneous abortion rate of surgical intervention during the first trimester and to avoid preterm labour when surgery occurs during the third trimester. This experience has not been reproduced in more recent literature reporting on laparoscopic cases [7]. Several studies showed that pregnant patients may undergo laparoscopic surgery safely during any trimester without any appreciated increased risk to the mother or fetus [10,11]. Although specific recommendations have been introduced [7,8], laparoscopic surgery during pregnancy is more difficult and should be reserved for experienced surgeons able to reduce the additional risks and operating time. Most likely, this is the key to the success of the surgical procedure and of the maternal-fetal well-being.
Acknowledgments
There are no acknowledgments
Disclosure
The author reports no conflicts of interest in this work
References
- osta-Martins S, Santos JV, Bernardes J (2016) Laparoscopic surgery during pregnancy. A survey among European Obstetricians and Gynecologists. Eur J Obstet Gynecol Reprod Biol 206: 247-248.
- Pearl J, Price R, Richardson W, Fanelli R (2011) Society of American Gastrointestinal Endoscopic Surgeons. Guidelines for diagnosis, treatment, and use of laparoscopy for surgical problems during pregnancy. Surg Endosc 25: 3479-3492.
- Kammerer WS (1979) Nonobstetric surgery during pregnancy. Med Clin North Am. 63: 1157-1164.
- Estadella J, Español P, Grandal B, Gine M, Parra J (2017) Laparoscopy during pregnancy: Case report and key points to improve laparoscopic management. Eur J Obstet Gynecol Reprod Biol 217: 83-88.
- Tsai HC, Kuo TN, Chung MT, Lin MY, Kang CY, et al. (2015) Acute abdomen in early pregnancy due to ovarian torsion following successful in vitro fertilization treatment. Taiwan J Obstet Gynecol 54: 438-441.
- Rackow BW, Patrizio P (2007) Successful pregnancy complicated by early and late adnexal torsion after in vitro fertilization. Fertil Steril 87: e9-e12.
- Yumi H (2008) Guidelines for diagnosis, treatment, and use of laparoscopy for surgical problems during pregnancy: This statement was reviewed and approved by the Board of Governors of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), September 2007. Surg Endosc 22: 849-861.
- Committee on Obstetric Practice and the American Society of Anesthesiologists (2017). Committee Opinion No. 696: Nonobstetric Surgery During Pregnancy. Obstet Gynecol 129: 777-778.
- 9 Munshi S, Patel A, Banker M, Patel P (2014) Laparoscopic detorsion for bilateral ovarian torsion in a singleton pregnancy with spontaneous ovarian hyperstimulation syndrome. J Hum Reprod Sci 7: 66-68.
- Oelsner G, Cohen SB, Soriano D, Admon D, Mashiach S, et al. (2003) Minimal surgery for the twisted ischaemic adnexa can preserve ovarian function. Hum Reprod 18: 2599-2602.
- Reedy MB, Källen B, Kuehl TJ (1997) Laparoscopy during pregnancy: a study of five fetal outcome parameters with use of the Swedish Health Registry. Am J Obstet Gynecol 177: 673-679.
- Wilasrusmee C, Sukrat B, McEvoy M, Attia J, Thakkinstian A (2012) Systematic review and meta-analysis of safety of laparoscopic versus open appendicectomy for suspected appendicitis in pregnancy. Br J Surg 99: 1470-1478.
- Walsh CA, Tang T, Walsh SR (2008) Laparoscopic versus open appendicectomy in pregnancy: a systematic review. Int J Surg 6: 339-344.
- Koo YJ, Kim HJ, Lim KT (2012) Laparotomy versus laparoscopy for the treatment of adnexal masses during pregnancy. Aust N Z J Obstet Gynaecol 52: 34-38.
- Rollins MD, Chan KJ, Price RR (2004) Laparoscopy for appendicitis and cholelithiasis during pregnancy: a new standard of care. Surg Endosc 18: 237-41.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences