Intrapartum Maternal Haemoglobin: A Predictor of Fetal Distress, Mode of Delivery, and Short-Term Neonatal Outcome in a Tertiary Care Hospital
Neha Garg*
Neha Garg*
Department of Obstetrics and Gynaecology, JJM Medical College, Davangere, Karnataka, India
- *Corresponding Author:
- Neha Garg
Junior Resident, Department of Obstetrics and Gynaecology
JJM Medical College, Davangere, Karnataka, 577004, India
Received date: April 20, 2020; Accepted date: April 27, 2020; Published date: May 15, 2020
Citation: Garg N (2020) Intrapartum Maternal Haemoglobin: A Predictor of Fetal Distress, Mode of Delivery, and Short-Term Neonatal Outcome in a Tertiary Care Hospital. Crit Care Obst Gyne Vol.6 No.2:15.
Abstract
Background: During pregnancy, the fetal stores for any nutrient are dependent on the maternal’s status for that nutrient. Maternal anaemia is associated with adverse birth outcomes along with maternal morbidity and mortality respectively. Similarly, elevated Hb levels may lead to diminished fetal and placental nutrient and oxygen supply resulting subsequently in fetal, placental, and maternal complications.
Objective: To explore (a) the relationship between event of fetal distress during term labour and intrapartum maternal haemoglobin level; (b) the relationship between mode of delivery, the reason for instrumental delivery and short-term neonatal outcome with maternal haemoglobin; and (c) Identify the factors influencing maternal haemoglobin level during the intrapartum period.
Results: Data of 7173 patients were analysed. Intrapartum Hb did not contribute to the prediction of the likelihood of fetal distress, IVD for non-progressive labour, CS for fetal condition, 5-min Apgar score <7, and pHa ≤ 7.05. However, there was a unique statistically significant contribution of Hb to the prediction of the likelihood of IVD for any reason and IVD for fetal distress and CS for any reason and CS for non-progressive labour. IVD for fetal distress was related to a higher intrapartum Hb level, whereas CS for non-progressive labour was related to a lower intrapartum Hb level. Factors identified to influence the intrapartum Hb level were maternal age, ethnicity, parity, fetal sex, and birth weight.
Conclusion: The risk of fetal distress and the adverse neonatal outcome is not correlated to intrapartum Hb levels. However, on the other hand, our data suggest that intrapartum Hb is a detrimental factor for a mode of delivery.
Keywords: Maternal haemoglobin; Fetal distress; Instrumental delivery; Neonatal outcome; Obstetric labour
Keywords
Maternal haemoglobin; Fetal distress; Instrumental delivery; Neonatal outcome; Obstetric labour
Introduction
In pregnancy, a woman undergoes various physiological adaptive changes. There is a disproportionate increase in plasma and Red Blood Cell volume which produces a state of hemodilution or physiological anaemia of pregnancy and it becomes more apparent at 30-34 weeks of gestation respectively [1,2].
Haemoglobin (Hb), an iron-containing conjugated protein present in the red blood cells of the blood is responsible for carrying oxygen to various tissues of our body. It’s value less than 11 g/dl is defined as ‘Anaemia in pregnancy’ by the World Health Organization [3]. Anaemia is a global problem. Its prevalence in India is about 60% and may increase to 80% during pregnancy. Nutritional anaemia especially due to iron deficiency is the most commonly seen in our setup of rural India [4]. Its incidence ranges from 35%-75% in developing countries and 18% in the developed world [5]. The risk factors for anaemia in pregnancy include low socioeconomic status, inadequate antenatal care, multiparity, and birth spacing <2 years [6-10].
Adverse outcomes of birth and maternal morbidity and maternal mortality can occur as a complication of maternal anaemia [11,12]. Similarly, elevated Hb levels may lead to diminished fetal and placental nutrient and oxygen supply and subsequently fetal, placental, and maternal complications [13,14].
Preplacental hypoxia can occur during pregnancy due to maternal anaemia [15]. The Hb levels at intrapartum phase influence fetal oxygenation and if compromised then it culminates into perinatal asphyxia. The state of perinatal asphyxia has been recognised as one of the main causes of neonatal morbidity and mortality [16]. And further will add on the risk of fetal distress during labour. Not many studies have been done to prove this hypothesis [17]. It may impede maternal endurance during labour and may also increase the risk of nonspontaneous delivery and cesarean section. Prior studies on its perinatal outcomes outline variable consequences [11-14,18].
The current trend advocates prenatal care, which is governed by principles of preventive obstetrics. Therefore, the factors responsible for anaemia and elevated haemoglobin in pregnancy should be identified and eradicated. And henceforth additionally outlines the significance of undertaking this study.
Objective
• To explore the relationship between the occurrence of fetal distress during term labour and intrapartum maternal haemoglobin level
• To explore the relationship between mode of delivery, the reason for instrumental delivery and short-term neonatal outcome and maternal haemoglobin
• To identify factors influencing intrapartum maternal haemoglobin level
Materials and Methods
With level IV evidence, a retrospective cohort study was performed from September 2017 to August 2018 in the department of Obstetrics and Gynaecology, Bapuji hospital, Chigateri Government General hospital, Women, and Child Health hospital attached to JJM Medical College, Davangere, Karnataka, India. The patients were recruited by a convenient sampling technique. A total of 7173 gravidas with term gestation upon fulfilling the inclusion and exclusion criteria were considered for the study.
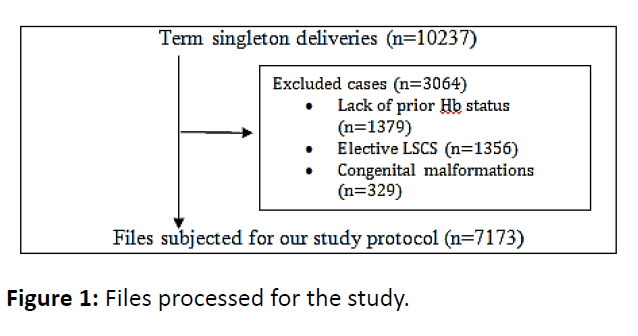
Women with term labour and women with living singleton fetus in cephalic presentation without congenital malformations were included for the study. These subjects had Hb reports of less than two weeks before delivery available. Women scheduled for elective cesarean section, women with haemoglobinopathies and patients refused participation as per our protocol were excluded from the study (Figure 1).
Working definitions in this study
• Normal Hb: 11.0 g/dl-12.9 g/dl
• Anaemia: Hb <11.0 g/dl
• Severe Anaemia: Hb <7.0 g/dl
• High Hb: Hb >12.9 g/dl; accordingly to other studies [13]
• Fetal distress: defined as ominous suspicion of fetal hypoxia determined by an abnormal FHR pattern as per the modified FIGO criteria [19]; Fetal Scalp Blood (FSB) pH <7.20 or significant ST-event [3]
• Mode of Delivery: Instrumental Vaginal Delivery (IVD), and Caesarean Section (CS) were categorized into three groups- IVD/ CS for fetal distress, IVD/ CS for non-progress of labour and IVD/ CS for any other reason
Statistical analysis
Analysis of data done using SPSS (version 24.0, IBM, Chicago, IL, USA). Hb served as a continuous value throughout analyses. Hb distribution assessed for normality; visually by the use of histograms and extreme outliers in a box plot, and mathematically by checking for values of skewness and kurtosis between -1 and +1. Hb was normally distributed. The maternal age and fetal birth weight were evaluated as continuous data. Univariate analysis with independent t-tests was used for the calculation of differences in mean Hb between several demographic, obstetric, and outcome variables. Pearson’s R was used to correlate Hb to continuous variables.
We selected continuous variables to be included in multiple regression analysis if they are significantly correlated to Hb (p<0.05), and categorical variables if mean Hb levels were significantly different between groups with or without a certain condition (p<0.05). Linear regression analysis was utilised to define the unique contribution of each of the independent variables on the intrapartum Hb level. Also, a logistic regression model was constructed for assessing influencement of Hb on the delivery outcome and identifying possible confounders. Odds ratios and 95% confidence Intervals (CI) were computed.
Results
During the study period, the singleton deliveries with term pregnancy were 10,237 respectively. A total of 3064 cases were excluded from the study as mentioned in Table 1. Following exclusion, a total of 7173 files were analysed finally.
| Variables | Pearson’s R correlation | Independent student’s t-test | p-value |
|---|---|---|---|
| Maternal age | 0.04 | <0.01 | |
| Parity | 12.78 | <0.01 | |
| Fetal sex | 2.71 | <0.01 | |
| Birth weight | - 0.13 | <0.01 | |
| 5 min APGAR score | 1.79 | 0.13 | |
| Fetal distress | 3.24 | <0.01 | |
| IVD for fetal distress | 2.81 | <0.01 | |
| IVD for non-progressive labour | 4.35 | <0.01 | |
| CS for fetal condition | -1.83 | 2.19 | |
| CS for non-progressive labour | -2.76 | 0.01 | |
| pH a ≤ 7.05 or >7.05 | 2.15 | 0.02 |
Table 1: Relationship between variables and mean haemoglobin level.
The study population existed of 4812 primiparous women (67.08%), mean age 29.41 ± 3.71 years (range: 15-52 years), and 341 neonates (4.75%) had a birth weight <2500 grams. The mean Hb concentration at admission was 11.71 ± 2.14 g/dL (range: 7.7-16.4). Intrapartum Hb concentration was low in 1700 (23.69%) women, normal in 3317 (46.24%) women, and high in 2156 (30.05%) women. No women were found to have severe anaemia. In 2341 deliveries, fetal distress was diagnosed (32.63%), in 42% of these deliveries an instrumental delivery was performed. In 407 cases, fetal distress was proven by FSB or an ST event (17.38%).
Relationship between demographic characteri- -stics and outcome variables and maternal Hb
Positive correlation between Hb and maternal age (r=0.04, p=0.05) and a negative correlation between Hb and fetal birth weight (r=-0.13, p=<0.01) was established. The mean Hb significantly varied between Indian and non-Indian women, primiparous and multiparous women. However, no variation in mean Hb value among women having a male or female fetus. The mean Hb levels varied significantly between the groups of women with complicated labour due to fetal distress, in comparison to the group of women delivering a fetus under a reassuring condition.
Also, mean Hb levels varied significantly between women who had an IVD for fetal distress, who had an IVD for nonprogressive labour, and who had a CS for nonprogressive labour, compared with the groups where these specific assisted-delivery measures were not undertaken (Table 1). The absolute difference in mean Hb levels was found to be 0.1 g/ dl-0.5 g/dL respectively.
Risk of fetal distress in relation to maternal Hb level
Initially, Hb levels were found to be significantly different between the groups where fetal distress was present or absent. Logistic regression was performed to assess the influence of the confounders. The model contained independent variables such as Hb, maternal age, parity, ethnicity, and birth weight), selected from the univariate analyses if p<0.05. Three variables such as age, parity, and birth weight made a unique statistically significant contribution to the model, indicating that after correction for these possible confounders. The strongest predictor of the occurrence of fetal distress was parity, recording an odds ratio of 0.49 (95% CI 0.41-0.55). This indicated that fetal distress was 0.49 less likely to occur in multiparous women when compared to primiparous women.
Relationship between mode of delivery, the reason for instrumental delivery and shortterm neonatal outcome and maternal Hb
The Hb level did not contribute to the prediction of the likelihood of IVD for non-progressive labour, CS for fetal condition, 5-min Apgar score <7, and pHa 7.05 which were found in repeated logistic regression analysis. There was a unique statistically significant contribution of Hb for the prediction of IVD for any reason, IVD for fetal distress, CS for any reason, and CS for non-progressive labour (Table 2). As there is an increment in Hb level by 1 g/dL, women were at 1.10 times more likely to have an IVD for any reason and for fetal distress. In contrast, for an increment in Hb level by 1 g/dL, the likelihood of having a CS for any indication or nonprogressive labour was 0.91 and 0.89, respectively.
| Outcome parameter | Standardised beta | Standard error | 95% CI | p-value |
|---|---|---|---|---|
| IVD | 0.00 | 0.02 | 1.05-1.91 | 0.00 |
| IVD for foetal distress | -0.01 | 0.05 | 1.04-1.43 | 0.05 |
| CS | 0.10 | 0.04 | 0.73-0.91 | <0.01 |
| CS for non- progressive labour | 0.12 | 0.03 | 0.89-0.99 | 0.01 |
Table 2: Multiple logistic regression analysis with the haemoglobin as a predicting factor for the likelihood of non-spontaneous delivery.
Factors influencing intrapartum maternal Hb level
Linear regression was appointed to assess the ability of two demographic variables (age, and parity) and two fetal variables (sex and birth weight) for predicting intrapartum Hb levels. All the variables had a significant contribution in predicting Hb level according to univariate regression analysis and forward linear regression analysis (Table 3), with parity accounting as a unique contribution to the model (Standardized Beta 0.15).
| Independent variable | Standardized beta | 95% CI | p-value |
|---|---|---|---|
| Parity | 0.15 | 0.29-0.42 | <0.01 |
| Maternal age | 0.13 | 0.02-0.03 | <0.01 |
| Birth weight | -0.16 | 0.33-0.51 | 0.03 |
| Fetal sex | 0.04 | 0.09-0.17 | 0.05 |
Table 3: Multiple variate regression analysis with intrapartum Hb as the dependent variable.
Discussion
Till date the imperative oxygen’s role in fetal development is controversial. Early embryogenesis occurs under anaerobic conditions; thereby it has no major role in the early gestational period. However, with advancing gestation oxygen becomes important for normal fetal organogenesis and growth (during 2nd and 3rd trimesters) [20]. The amount of oxygen in the mother’s blood and thus available for the fetus is determined by the maternal Hb value. In pregnancy, the optimum Hb levels are 11 g/dl-12.9 g/dl and value lesser than 11, and more than 12.9 both have adverse pregnancy and perinatal outcomes.
Anaemic patients may not tolerate even normal blood loss during delivery and lead to complications such as postpartum haemorrhage. Anemic women may not be able to endure natural process of labour; increasing the incidence of instrumental and caesarean deliveries for such women. Awasthi A et al. [9] reported an incidence of 2.5% of PPH and of 2.09% of retained placenta. 20.5% and 6.5% of anemic women had caesarean and instrumental delivery as opposed to 5% and 2% in normal women respectively. 69.5% anemic vs 89% normal women had a normal vaginal delivery. Maternal morbidity with the incidence of congestive cardiac failure (23.07%), subinvolution of uterus (2%), wound dehiscence (2.45%), fever (8.6%) spikes in anemic population. Brabin BJ et al. [12] stated the estimated maternal mortality from anaemia to be around 27 per 1,00,000 live births in India. Also, high Hb values were associated with slightly upscale mortality risk.
There is a high incidence of adverse fetal outcomes in the form of preterm birth, IUGR, stillbirths, low birth weights, birth asphyxia, early neonatal deaths in the anemic group compared to controls. Awasthi A et al. [9] and Rangnekar AG et al. [6] reported higher incidences of preterm birth (9.5%; 73%), IUGR (37.5%; 1%), and stillbirth (6.5%; 15%) respectively in anaemic women. A study of 629 women done in Pakistan [11] in 2004 revealed the underlying risk of preterm delivery and Low Birth Weight (LBW) babies, APGAR score <5 at 1 min, and IUD was 4, 1.9, 1.8 and 3.7 times more among anaemic women, respectively. Drukker L et al. [18] in 2015 on studying 75,660 deliveries inferred that iron deficiency anaemia at delivery paves the way to increased risk for caesarean section, adverse maternal and neonatal outcomes in otherwise healthy women.
Sekhavat L et al. [21] concluded that anaemia (Hb<10 g/dl) was associated with increased risk of LBW and low APGAR score significantly. Furthermore, high Hb (>13 g/dl) also increased the risk of LBW, however, regarded insignificant. An analysis of 153602 pregnant women with various ethnic groups in 1995 [14] showed a striking U shaped distribution of the rate of low birth weight by Hb group with the incidence of low birth weight being least at 96 g/dl-105 g/l. Gaillard R et al. [13] in 2014 showed that elder maternal age, higher body mass index, primiparity, European descent were associated with higher Hb levels (p<0.05). This, in turn, was associated with shooting up of systolic and diastolic blood pressures throughout the gestational period. Also, posing a higher risk of uterine artery notching, gestational hypertensive disorders along with fetal head circumference, length and weight growth restriction from third trimester onwards (p<0.05) culminating into adverse birth outcomes. Thence, high Hb level and absence of haemoglobin dilution during pregnancy could be regarded as an indicator of high-risk pregnancy. A study done in Northern Iran [22] in 2016 revealed that the elevated maternal Hb during pregnancy accounts as a risk factor for stillbirth and further low Hb level had an inverse relation with stillbirth.
A recent study was done by Bullens LM et al. [17] analysed data on 9144 patients is at par with our current study which concluded that intrapartum Hb did not contribute to the prediction of the likelihood of fetal distress, instrumental vaginal delivery for nonprogressive labour, caesarean section for fetal conditions and 5 min APGAR score<7. But, there was a unique statistically significant contribution of Hb to the prediction of the likelihood of instrumental vaginal delivery for any reason and fetal distress and caesarean section for any reason and for non-progressive labour. IVD for fetal distress was related to a higher intrapartum Hb level, whereas CS for non-progressive labour was related to lower intrapartum Hb. Intrapartum Hb was influenced by maternal age, ethnicity, parity, fetal sex, and birth weight.
Conclusion
Our study concludes that intrapartum Hb levels determine the mode of delivery. On the contrary, the chances of fetal distress and the subsequent unfavourable neonatal outcome are independent of intrapartum Hb levels. Thus, intrapartum Hb levels in women near term can play a pivotal role in deciding delivery mode beforehand for optimal maternal and perinatal outcomes.
Funding Sources
Nil
Conflict of Interest
Nil
Acknowledgement
Nil
References
- Dutta DC (2018) Physiological changes during pregnancy (9th ed.). Jaypee Brothers, pp: 42-52.
- Bernstein IM, Ziegler W, Badger GJ (2001) Plasma volume expansion in early pregnancy. Obstet Gynecol 97: 669-674.
- World Health Organization (2015) The global prevalence of anemia in 2011: Geneva.
- Matah M, Mukherjee P, Matah A, Matah P. Anaemia in pregnancy. In: Principles and practice of obstetrics and gynecology (Chapter 7. 3rd edn). Jaypee Publications, pp: 69-99.
- Lindsay HA (2000) Anemia and iron deficiency: effects on pregnancy outcome. Am J Clin Nutr 71: 1280S-1284S.
- Rangnekar AG, Darbari R (1993) Fetal outcome in pregnancy anemia. J Obstet Gynecol India 43: 172-176.
- Thangaleela F, Vijayalakshmi P (1994) Impact of anaemia in pregnancy. The Ind J Nutr Dietet 31: 251-256.
- Khandail WD, Ambadckar NN, Zodpey PS, Koram MR, Vasudeo ND (2001) Risk factors for anaemia in pregnancy. J Obstet Gynecol India 51: 42-44.
- Awasthi A, Thakur R, Dave A, Goyal V (2001) Maternal and perinatal outcome in cases of moderate and severe anemia. J Obst Gyn India 51: 62-65.
- Alli R, Satyanarayana M (1985) Anemia complicating pregnancy. J Obstet Gynecol India 35: 335-338.
- Lone FW, Qureshi RN, Emanuel F (2004) Maternal anaemia and its impact on perinatal outcome. Trop Med Int Health 9: 486-490.
- Brabin BJ, Hakimi M, Pelletier D (2001) An analysis of anemia and pregnancy-related maternal mortality. J Nutrition 131: 604S-614S.
- Gaillard R, Eilers PHC, Yassine S, Hofman A, Steegers EAP, et al. (2014) Risk factors and consequences of maternal anaemia and elevated haemoglobin levels during pregnancy: a population based prospective cohort study. Paediatr Perinat Epidemiol 28: 213-226.
- Steer P, Alam MA, Wadsworth J, Welch A (1995) Relation between maternal haemoglobin concentration and birth weight in different ethnic groups. BMJ 310: 489-91.
- Kingdom JCP, Kaufmann P (1997) Oxygen and placental villous development: origins of fetal hypoxia. Placenta 18: 613-621.
- Lawn JE, Cousens S, Zupan J (2005) 4 million neonatal deaths: when? Where? Why? Lancet 365: 891-900.
- Bullens LM, Smith JS, Truijens SEM, Jagt MBH, Heimel PJR, et al. (2019) Maternal haemoglobin level and its relation to fetal distress, mode of delivery, and short-term neonatal outcome: a retrospective cohort study. J Matern Fetal Neonatal Med 31: 1-7.
- Drukker L, Hants Y, Farkash R, Ruchlemer R, Samueloff A, et al. (2015) Iron deficiency anemia at admission for labor and delivery is associated with increased risk for caesarean section and adverse maternal and neonatal outcomes. Transfusion 55: 2799-2806.
- Ayres-de-Campos D, Spong CY, Chandraharan E (2015) For the FIGO intrapartum fetal monitoring expert panel. FIGO consensus guidelines on intrapartum fetal monitoring: cardiotocography. Int J Gynecol Obstet 131: 13-24.
- Hutter D, Kingdom J, Jaeggi E (2010) Causes and mechanisms of Intrauterine hypoxia and its impact on the fetal cardiovascular system: a review. Int J Pediatr 2010: 401323.
- Sekhavat L, Davar R, Hosseinidezoki S (2011) Relationship between maternal haemoglobin concentration and neonatal birth weight. Hematology 16: 373-376.
- Maghsoudlou S, Cnattingius S, Stephansson O, Aarabi M, Semnani S, et al. (2016) Maternal haemoglobin concentrations before and during pregnancy and stillbirth risk: a population-based case-control study. BMC Pregnancy Childbirth 16: 135.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences