Evaluation of Postpartum Blood Loss After Misoprostol-Induced and Oxytocin with Foley's Catheter-Induced Labour: A Comparative Study
Neha Garg and Vanitha VG
Neha Garg* and Vanitha VG
Department of Obstetrics and Gynaecology, JJM Medical College, Davangere, Karnataka, India
- *Corresponding Author:
- Neha Garg
Junior Resident, Department of Obstetrics and Gynaecology
JJM Medical College, Davangere, Karnataka, 577 004, India
Received date: February 3, 2020; Accepted date: February 7, 2020; Published date: February 15, 2020
Citation: Garg N, Vanitha VG (2019) Evaluation of Postpartum Blood Loss After Misoprostol-Induced and Oxytocin with Foley’s Catheter- Induced Labour: A Comparative Study. Crit Care Obst Gyne Vol.6 No.1:12.
Keywords
Misoprostol; Foley’s catheter; Oxytocin; Labor induction; Postpartum blood loss
Abstract
Background: Among the reported adverse effects of labor induction, little has been documented about postpartum bleeding. In our population where anemia is a common problem, any significant amount of blood loss beyond what the individual may be able to tolerate may compromise hemodynamic status resulting in additional therapy, with increased healthcare costs. The best agent and method for the induction of labor remains uncertain. Objective: To evaluate and compare postpartum vaginal blood loss and efficacy of the combination of Foley's bulb and oxytocin with vaginal misoprostol alone for labor induction. Materials and Methods: A total of 200 pregnant women were randomized into two groups of 100 each for misoprostol (Group M-50 µgram intravaginal) or Foley's catheter with oxytocin (Group FO) as methods of induction. Blood loss was measured using a plastic collection bag and weighing of the pads up to 6 hours postpartum. Pre- and post-delivery hemoglobin (Hb) and hematocrit (HCT) were measured and differences assessed and analyzed. The main outcomes measured were the success of induction, induction-delivery interval, postpartum blood loss, and difference between pre- and post-delivery Hb and HCT levels. The analysis was done with IBM SPSS version 24.0 for windows. Results: Age, parity, gestational age, episiotomy, and perineal tears were comparable in both groups. The mean blood loss in group M (60.52 ± 54.68 g) was significantly higher than group FO (36.94 ± 27.79 g) (p=0.00). The differences between mean pre-delivery Hb and HCT levels (12.23 ± 1.32 g/dl; 38.18 ± 3.01% and 12.35 ± 1.31 g/dl; 38.25 ± 3.31% in group M and group FO respectively) and post-delivery Hb and HCT (10.53 ± 1.45 g/dl; 34.55 ± 4.22% and 10.45 ± 1.32 g/dl; 34.58 ± 4.15% in respective groups) were comparable between both groups. This difference was statistically insignificant (p>0.05). Whereas, within each group, pre and post-delivery Hb and HCT level differences were statistically highly significant (p=0.001). A mild positive correlation between postpartum blood loss and initial Bishop scores and induction delivery interval was seen in group FO as compared to no such correlation in group M. Induction to the delivery interval was shorter in group FO (11.43 ± 5.25 hours vs 12.49 ± 5.62 hours) (p=0.169). Conclusion: Induction with Foley's catheter with sequential use of oxytocin was found to be more efficacious as compared to intravaginal misoprostol for labor induction
Introduction
The process of labor should be given to operating on its own and its spontaneous onset is most desirable and effective. Interference with this natural process, i.e. Induction of labor is one of the most important interventions in obstetrics, the epidemiology of which has changed over the years, with the continued rise of its incidence [1]. It should be done if its benefits outweigh the potential harm both for the mother and her unborn child [2].
Various methods of ripening of the cervix and induction of labor are being used by obstetricians including intravenous infusion of oxytocin, intravaginal or intracervical administration of prostaglandins (PGE2 and PGE1) and intracervical Foley’s catheter insertion.
In induction of labor, the reported adverse effects are; increased bleeding, uterine hyperstimulation and rupture and fetal distress. However, little has been said about increased postpartum bleeding [3-5]. Postpartum bleeding appears to be quite relevant in our population where anemia is a common problem, as any significant amount of blood loss beyond what the individual may be able to tolerate, may compromise hemodynamic status resulting in additional therapy, with increased healthcare costs. The best agent and method for the induction of labor remains uncertain [6,7]. There is a paucity of data on prospective postpartum blood loss evaluation following labor induction. Thus, the need for this study.
Objective
To evaluate and compare postpartum vaginal blood loss and efficacy of the combination of Foley’s bulb and oxytocin with vaginal misoprostol alone for labor induction.
Materials and Methods
With level IV evidence, a prospective comparative study was performed from October 2017 to September 2019 in the department of Obstetrics and Gynaecology, Bapuji hospital, Chigateri Government General hospital, Women and Child Health hospital attached to JJM Medical College, Davangere, Karnataka, India. A total of 200 cases were selected for the study and allocated into two groups namely Group 1: Induced with misoprostol (Group M) (n=100) and Group 2: Induced with Foley’s catheter followed by oxytocin (Group FO) (n=100).
Primigravida with term gestation of 37 completed weeks up to 41 completed weeks with a live singleton pregnancy with vertex presentation, intact membranes with no evidence of labor (Bishop score <5 using modified Bishop scoring) and no contraindications to vaginal delivery were included in the study. Women with non-vertex presentations, multiple pregnancies, pregnancy with bad obstetric history, women with medical disorders complicating pregnancy, women with thrombocytopenia and deranged coagulation profile and patients with seropositive cases of HIV and hepatitis B were excluded from the study.
Examination and detailed ultrasonography. Routine laboratory investigation with hemoglobin, hematocrit, blood indices, bleeding and clotting time was carried out.
Eligible women were randomized and open-labeled to the following groups:
a. Group M (Misoprostol Induction) (n=100): 50 μg of intravaginal misoprostol repeated 6th hourly until an adequate contraction pattern (3-5 contractions in ten minutes, each lasting 40-60 seconds), sufficient cervical ripening (bishop score>7 or cervical dilatation of at least 4 cm), or spontaneous rupture of membranes was achieved, or a maximum of 4 doses was given
b. Group FO (Oxytocin Induction after Ripening with Foley’s Catheter) (n=100): A size 18 Foley’s Catheter was inserted into the extra-amniotic space and the bulb inflated with 30 cm3 of saline/sterile water. It was taped under gentle traction to the inner aspect of the woman’s thigh. It was left in-situ until spontaneously expelled, but not exceeding 12 hours when the balloon will be deflated and the catheter removed. Then synchronous fore-water amniotomy and incremental intravenous oxytocin (10 mU/ml) titration were done. It was commenced at a rate of 10 drops per minute (6.67 mU/min) and titrated by increasing the rate by 10 drops every 30 minutes, until adequate contractions were established or till a maximum rate of 60 drops per minute (40 mU/min) was reached.
The mediolateral episiotomy was performed in all cases. Immediately after delivery of the baby, after draining off the liquor, the patient was placed over a blood drape-a disposable conical, graduated plastic collection bag. Blood loss was promptly read and recorded. Active management of the third stage of labor was carried out. Apgar scores of the baby at the first and fifth minute, birthweight, and NICU admissions were recorded. Women were transferred to the Postnatal ward approximately half an hour after placental delivery. Clean weighed pads were applied to evaluate blood loss in the following 6 hours. Repeat laboratory investigation with hemoglobin, blood indices, and hematocrit were carried out after 24 hours of delivery.
The parameters recorded were: induction-delivery interval, mode of delivery, maternal and neonatal complications, postpartum blood loss, its correlation with initial bishop score and induction-delivery interval and the difference between pre- and post-delivery hemoglobin and hematocrit in both induction groups.
The categorical variables were represented in the form of frequency and percentages. The association of variables was done using Chi-square test. Continuous variables were represented as mean and Standard Deviation. A comparison of mean between groups was done with Unpaired t-test. To know the relation between the variables within the group Pearson’s Correlation was done. The analysis was done with IBM SPSS version 24.0 for windows.
Results
A total of 200 patients were divided into two groups of 100 each with the method of induction being either misoprostol or Foley’s catheter followed by oxytocin.
The age distribution was comparable in both the groups (statistically insignificant, p=0.207). The maximum number of patients in each group belonged to the range of 20-29 years (Table 1). The majority of the cases in group M (70%) and group FO (83%) were full-term pregnancies. Post-dated pregnancies constituted up to 30% and 17% in respective groups. The difference between both groups was statistically significant (p=0.05).
| Age groups (Years) | Misoprostol Group M(n) |
Foley’s Group FO(n) |
Chi-square test | p-value |
|---|---|---|---|---|
| <20 | 12 | 5 | 3.152 | 0.207 |
| 20-29 | 78 | 84 | ||
| 30-39 | 10 | 11 | ||
| Total | 100 | 100 |
Table 1: Comparison of age distribution in both groups.
A total of 7% in group M and 86% in group FO had a spontaneous vaginal delivery. Instrumental delivery was seen in 7% and 5% and cesarean section in 6% and 9% in respective groups. This difference between both the groups in all the modalities of delivery was statistically insignificant (p=0.364).
Majority cases in both the groups had clear liquor (83% in group M and 91% in group FO). With misoprostol, 7 cases ended up having thick meconium and 10 having thin meconium. On the other hand, with Foley’s with oxytocin, there were respectively 4% and 5% cases out of the total. The differences between the groups were not statistically significant (p>0.680). The placenta was expelled completely in all cases in both groups. The mean induction to the delivery interval in group M was (12.49 ± 5.62) hours while in group FO it was (11.43 ± 5.25) hours (p>0.169).
The mean birth weight of babies delivered in group M and group FO was (2.93 ± 0.47) kg and (2.80 ± 0.42) kg respectively, which was statistically significant (p=0.03). In group M, 9% of the babies required NICU admissions for various complications as compared to 7% in group FO. This was statistically insignificant. No maternal complications were seen in any case.
The mean blood loss after misoprostol induction was (60.52 ± 54.68) g and after Foley’s with oxytocin, induction was (36.94 ± 27.79) g. The difference between both groups was statistically highly significant (p=0.000). The mean initial bishop score in the misoprostol group was (3.14 ± 1.42) and in Foley’s with oxytocin group, it was 1.83 ± 1.40. The difference was statistically highly significant (p=0.000).
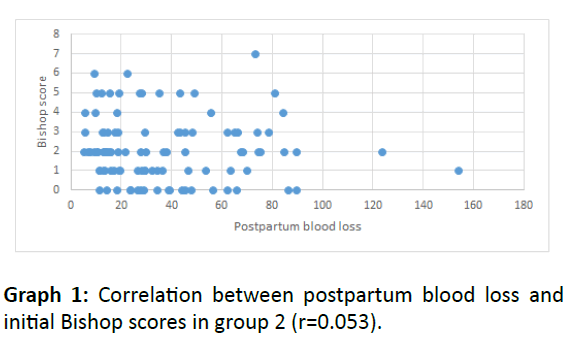
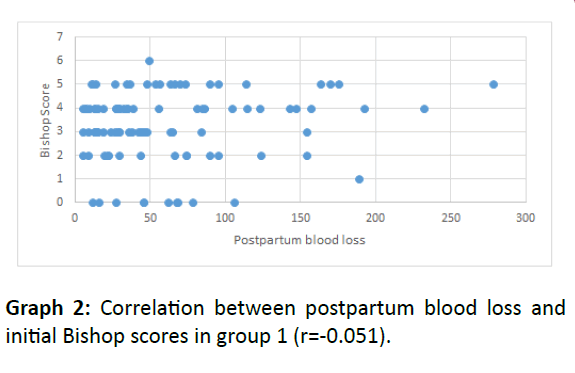
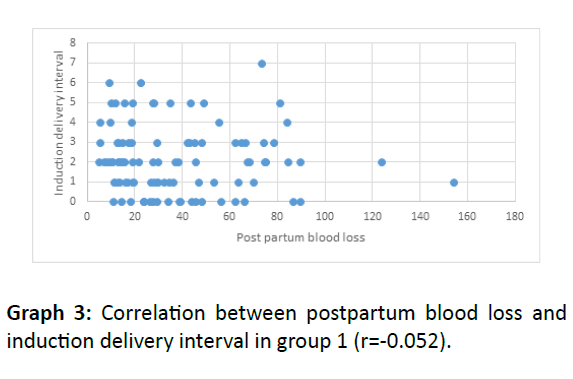
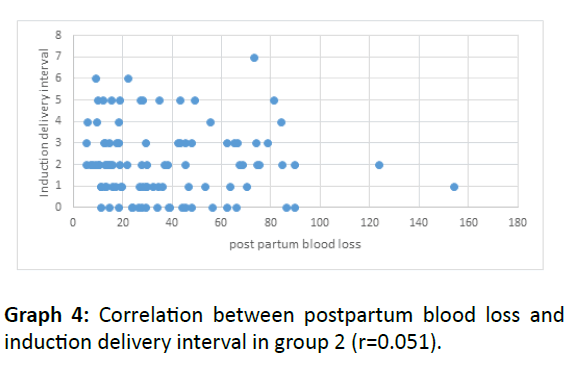
With misoprostol, mean pre- and post-delivery hemoglobin (Hb) level was (12.23 ± 1.32) g/dl was (10.53 ± 1.45) g/dl respectively. Similarly, in group FO the mean pre-delivery Hb was (12.35 ± 1.31) g/dl and post-delivery was 10.45 ± 1.32 g/dl. The mean hematocrit (HCT) values before delivery was (38.18 ± 3.01)% in group M and (38.25 ± 3.31)% in group FO. Similarly, the post-delivery HCT values were also comparable with (34.55 ± 4.22)% and (34.58 ± 4.15)% respectively. The difference between both groups was not statistically significant. However, within each group the difference between pre and post-delivery Hb and HCT was statistically highly significant (Graphs 1-4).
There is no correlation between postpartum blood loss and initial Bishop scores in the Misoprostol group (r=-0.051).
There is a mild positive correlation between postpartum blood loss and initial Bishop scores in Foley’s group (r=0.053).
There is no correlation between postpartum blood loss and induction delivery interval in the Misoprostol group (r=-0.052).
There is a mild positive correlation between postpartum blood loss and induction delivery interval in Foley ’s group (r=0.051).
Discussion
Does Induction of Labor (IOL) increase postpartum blood loss?
The analysis of the effect of IOL on blood loss following delivery has been controversial and poorly documented in the past. This is because of the other risk factors for increased blood loss after delivery could not be analyzed. As per previous studies done by Phillip et al. [5] IOL (irrespective of the method used) was associated with significantly greater mean blood loss at delivery as compared to spontaneous labor (SOL). It was also independently directly associated with placental weight, fetal birth weight, and length of the third stage of labor, but not the length of the first stage of labor [5]. Similarly, Khireddine et al. [8] and Sheldon et al. [9] suggested women with IOL following a standard indication were at a higher risk of postpartum hemorrhage (PPH). On the other hand, studies by Souza et al. [10] and Brun et al. [11] concluded that IOL is not associated wi5th increased blood loss after delivery. It was even associated with a minimal, however statically significant, reduced decrease in hemoglobin after delivery as compared to SOL.
In the present study, age, parity, gestational age at delivery, birth weight, episiotomy, perineal tear frequency and management of the third stage of labor were comparable between the two groups. The mean age of the participants was (24.68 ± 3.95) years in group M and (24.46 ± 3.42) years in group FO. The only primigravida was included in our study due to the known implication of multiparity being associated with a reduced decrease in hemoglobin due to a shorter second stage of labor and faster deliveries. The mean birth weight of babies delivered in group M was (2.93 ± 0.47) kg and in the group, FO was (2.80 ± 0.42) kg. Therefore, all confounding factors, which could individually affect the blood loss were eliminated. These findings were in conformity with that of Okon et al. [3], Elsedeek et al. [4] and Fox et al. [12].
Comparison of postpartum blood loss
In our study, blood loss in group M ranged between (56.82 to 64.59) g (mean-60.52 ± 54.68 g) which was significantly higher than in group FO with a range of 34.17 g to 39.01 g (mean 36.94 ± 27.79 g). Excessive blood loss in the misoprostol group could be explained by the possibility of obviation of adequate expression of regulatory molecules and excessive cervical and lower segment collagenolysis [4] resulting in excessive fragility of tissues interfering with retraction needed for arresting blood loss. This was consistent with the findings of Okon et al. [3] (488 ± 222) ml in the former group, (326 ± 106) ml in the later group; p=0.002). Elsedeek et al. [4] concluded that blood loss postpartum after misoprostolinduced labor (290 ml to 1200 ml with mean of 573 ± 208 ml) was significantly higher than with oxytocin induction (190 ml and 800 ml; mean 473 ± 155 ml). Phillip H et al. [5] concluded that PPH was highest with misoprostol (5.8%) versus 4.4% for spontaneous labor, 1.1% for oxytocin and none for the combined (misoprostol with oxytocin) category. Studies done on the use of oxytocin during labor goes on to show that it can be an independent risk factor for severe PPH as shown by Belghiti et al. [13].
Comparison of blood indices (Haemoglobin and Haematocrit)
No statistically significant difference was seen between pre and post-delivery Hb and HCT when comparing both groups. But within respective groups, the differences in the blood indices (Hb, HCT) were statistically highly significant. Similarly, Souza PC et al. [10] showed significant differences between pre- and postpartum Hb levels (p<0.0001) in cases of misoprostol-induced vaginal deliveries, non-induced vaginal deliveries, cesarean sections after attempted misoprostol induction and elective cesarean sections. But these differences were found to be proportional between all the groups. On the other hand, Elsedeek et al. [4] found a difference between preand post-delivery HCT was significantly larger with misoprostol.
Comparison of correlation of postpartum blood loss with other variables
In this study, no correlation between postpartum blood loss with initial Bishop scores and with induction delivery interval was found in group M. However, there was a mild positive correlation between the same variables in group FO. This is, in contrast, to study done by Elsedeek et al. [4] which found a significant positive correlation between postpartum blood loss and initial bishop score, and significant negative correlation between the same variable and duration of labor in both misoprostol and oxytocin-induced groups. Okon et al. [3] showed a significant positive correlation between postpartum blood loss and induction-delivery interval. However, there was no conclusive significant correlation between the former variable and the initial bishop score among both groups similar to our study.
Group FO (with initial bishop score of 1.83 ± 1.40 vs 3.14 ± 1.42, p<0.05) was associated with shorter induction-delivery time as compared to misoprostol (11.43 ± 5.25 hours vs 12.49 ± 5.62 hours, p>0.05). Culver et al. [14] also showed similar results. Contrasting results were found in studies by Okon et al. [3] Elsedeek et al. [4] and Moraes Filho OB et al. [15]. The labor complications and foetal outcomes were similar in studies done by Fox N et al. [12] Culver et al. [14] Filho et al. [15] and Owolabi et al. [16] However, later study showed misoprostol to be associated with tachysystole and hyperstimulation with none reported in ours.
Conclusion
Induction with Foley ’ s catheter with sequential use of oxytocin, when compared to intravaginal misoprostol is a more effective alternative for labor induction. This modern method of induction shall go a long way for its ability to induce labor and its favorable outcomes.
References
- WHO recommendations for induction of labour (2011) World Health Organization: Geneva.
- American College of Obstetrician and Gynecologist (ACOG): ACOG practice bulletin. (2009) Induction of labor. Obstet Gynecol 114: 386-397.
- Okon OA, Ekabua JE (2017) Postpartum vaginal blood loss following two different methods of cervical ripening. Obstet Gynecol Int 2017: 1-6.
- Elsedeek M, Awad E, Elsebaey S (2009) Evaluation of postpartum blood loss after misoprostol-induced labour. BJOG 116: 431-435.
- Phillip H, Fletcher H, Reid M (2004) The impact of induced labour on postpartum blood loss. J Obstet Gynecol 24: 12-15.
- Agan T, Ekabua J, Udoh A, Ekanem E, Efiok E, et al. (2010) Prevalence of anemia in women with asymptomatic malaria parasitemia at first antenatal care visit at the university of calabar teaching hospital, Calabar, Nigeria. Int J Womens Health 2: 229-233.
- Kirti Iyengar (2012) Early postpartum maternal mortality among rural women of Rajasthan, India: A community-based study. J Health Popul Nutr 30: 213-225.
- Khireddine I, Le Ray C, Dupont C, Rudigoz RC, Bouvier-Colle MH, et al. (2013) Induction of labour and risk of postpartum hemorrhage in low risk parturients. PLoS ONE 8: e54858.
- Sheldon WR, Blum J, Vogel JP, Souza JP, Gulmezoglu AM, et al. (2014) Postpartum haemorrhage management, risks, and maternal outcomes: findings from the world health organization multicountry survey on maternal and newborn health. BJOG 121: 5-13.
- Souza PC, Damasceno KS, Araujo Junior E, Alencar Junior CA, Feitosa FE (2017) Can the induction of labor with misoprostol increase maternal blood loss? Rev Bras Ginecol Obstet 39: 53-59.
- Brun R, Spoerri E, Schaffer L, Zimmermann R, Haslinger C (2019) Induction of labor and postpartum blood loss. BMC Pregnancy Childbirth 265: 1-7.
- Fox N, Saltzman D, Roman A, Klauser C, Moshier E, et al. (2011) Intravaginal misoprostol versus Foley catheter for labour induction: a meta-analysis. BJOG 118: 647-654.
- Belghiti J, Kayem G, Dupont C, Rudigoz RC, Bouvier-Colle MH, et al. (2011) Oxytocin during labour and risk of severe postpartum haemorrhage: a population-based cohort-nested case-control study. BMJ Open 1: e000514.
- Culver J, Strauss RA, Brody S, Dorman K, Timlim S, et al. (2004) A randomized trial comparing vaginal misoprostol versus Foley catheter with concurrent oxytocin for labor induction in nulliparous women. Am J Perinatol 21: 139-46.
- Moraes Filho OB, Albuquerque RM, Cecatti JG (2010) A randomized controlled trial comparing vaginal misoprostol versus foley catheter plus oxytocin for labor induction. Acta Obstet Gynecol Scand 89: 1045-1052.
- Owolabi AT, Kuti O, Ogunlola IO (2005) Randomized trial of intravaginal misoprostol and intracervical foley catheter for cervical ripening and induction of labor. J Obstet Gynecol 25: 565-568.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences