Effectiveness of Non-pneumatic Anti-shock Garment (NASG) in Preventing Shock-related Morbidity and Mortality in Severe Hemorrhagic Shock
Okafor I
DOI10.21767/2471-9803.1000149
Department of Obstetrics and Gynecology, Enugu State University of Science and Technology College of Medicine, Enugu State University Teaching Hospital, Enugu, Nigeria
- *Corresponding Author:
- Okafor I
Department of Obstetrics and Gynecology
Enugu State University of Science and Technology College of Medicine
Enugu State University Teaching Hospital, Enugu, Nigeria
Tel: +2348034006918
E-mail: okaforii@yahoo.com
Received date: June 12, 2017; Accepted date: June 20, 2017; Published date: June 27, 2017
Citation: Okafor II. Effectiveness of Non-Pneumatic Anti-Shock Garment (NASG) in Preventing Shock-related Morbidity and Mortality in Severe Hemorrhagic Shock. Crit Care Obst Gyne. 2017, 3:3. doi:10.21767/2471-9803.1000149
Copyright: © 2017 Okafor I. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Context: NASG is a first-aid-life-sustaining-device that supports the life of a patient in hemorrhagic shock during delays in receiving appropriate healthcare services by shunting blood from the lower body to the core organs.
Objectives: To reappraisal the effectiveness of NASG in sustaining life, and preventing shock-related morbidity and mortality during obstetric delays and make recommendations.
Method: The case notes of 4 patients that were managed with NASG in Enugu State University Teaching Hospital (ESUTH), Enugu from July 25, 2016 to April 3, 2017 were reviewed and the results presented in tables and percentages.
Results: The mean age and parity of the patients were 31.8 years and 3.5 respectively. They presented in severe hemorrhagic shock with 2/4 (50%) unconscious, 2/4 (50%) pulseless, and low mean arterial pressures. The two unconscious patients became conscious with the restoration of pulses on the application of NASG. The vital signs of the patients improved when the causes of shock were properly treated. Uterine rupture ¾ (75%), vaginal lacerations 1/4(20%) and cervical tear ¼ (25%) accounted for the hemorrhagic shock in this reappraisal. A total of 23 pints of blood were transfused. All the patients survived and none had shock-related morbidity.
Conclusions: This reappraisal has confirmed the effectiveness of NASG in preventing shock-related complications during obstetric delays. The causes of the shock must be identified and properly treated to optimize its effectiveness. NASG should be available in every childbirth center.
Keywords
NASG; Severe shock; Prevention; Morbidity; Mortality
Introduction
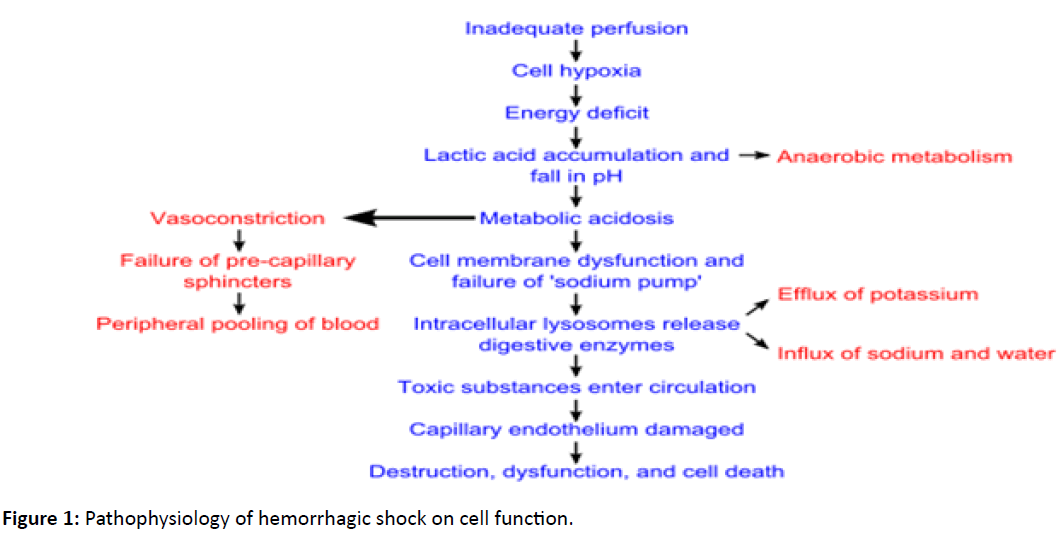
Postpartum hemorrhage (PPH) is known to account for 35% of all maternal deaths [1]. A woman suffering from PPH and hypovolemic shock can die within 2 hours unless she receives immediate blood transfusion and appropriate emergency obstetric care [2]. The knowledge of the pathophysiology of hemorrhagic shock as depicted in Figure 1 is critical for the understanding of the clinical features and classifications3-6 of shock (Table 1). Such a background paves the way for the understanding of the role of NASG demonstrated in Figure 2 in sustaining life when ‘delays’ occur in the management of hemorrhagic shock.
| Compensated | Decompensated | |||
|---|---|---|---|---|
| Stage 1 | Stage 2 | Stage 3 | Stage 4 | |
| Blood volume loss | <15% (<750 ml) | 15-30% (750-1,500 mL) | 30-40% (1,500-2,000 mL) | <40% (>2,000 mL)(immediately life threating) 2 |
| Cardiac output | Compensated by constriction vascular bed | lower | lower | lower |
| Systolic blood pressure | Normal | normal | <100mm Hg | <70 mm Hg |
| Diastolic blood pressure | Normal | increased | often not detectable due to narrow gap between syst and diast BP | |
| Respiratory rate | Normal | Increased (tachypnea) | >30 %/min | Pronounced tachynea |
| Heat rate | Slightly increased but <100/min | >100/min | >120/min | >140/min |
| Pulse | Normal | weak | weak | Weak or absent |
| Capillary refil | Normal (<2 sec) | Delayed (>2 sec) | Delayed (>2 sec) | Absent |
| Urine outout | Normal (>30 mL/hour) | 20-30 mL/hour | <20 mL/hour | Negligible |
| skin | pale | pale, sweaty | Cool, pale, sweaty | Cool, extremely, pale, sweaty |
| Mental status | Slightly anxiety | Slight anxiety, restlessness | Confusion, agitation | lethargy, coma |
Table 1: Clinical features and classifications of hypovolemic shock [3-6].
Hypovolemia and hypoperfusion of tissue cause cellular oxygen deficiency, anaerobic metabolism and lactic acidosis. Oxygen deficiency prevents the entry of pyruvate into the Krebs cycle and electron transport chain for massive production of Adenosine Triphosphate (ATP) as energy. The accumulated pyruvate is converted to lactate by lactate dehydrogenase thus causing lactic acidosis.
The body employs several compensatory physiological, neural, hormonal and biochemical mechanisms in an attempt to reverse the hypovolemic shock. The baroreceptors in the arteries detect the resulting hypotension, and cause massive sympathetic nervous system stimulation, and the release of epinephrine and norepinephrine. They cause widespread vasoconstrictions and tachycardia to increase blood pressure. The accumulated lactic acidosis causes hyperventilation to get rid of carbon dioxide in the body. The renin-angiotensin is activated, and anti-diuretic hormone is released to conserve fluid via the kidneys. These hormones also cause vasoconstriction of the kidneys, gastrointestinal tract, and other organs to divert blood to the heart, lungs and brain. This causes the characteristic low urine output in shock patients. Progressive shock stage occurs when the hemorrhage persists, and the compensatory mechanisms begin to fail. Metabolic acidosis causes cell membrane dysfunction, and sodium/potassium ion pump to fail. Sodium ions influx occurs within the cells with the accompanying by potassium ions efflux. As anaerobic metabolism continues, wide spread vasodilatations occur, and blood pools in the capillaries [3]. Increase in hydrostatic pressure and histamine release cause leakage of fluid and protein into the surrounding tissues causing increase in blood viscosity, micro-circulation occlusions, multiple organ dysfunctions and cell deaths. Ischemia of the bowel can cause bacteria to enter the blood stream, and may result in endotoxic shock [3,4].
At the refractory shock stage, the vital organs have failed and the shock becomes irreversible shock. Brain damage and cell death occur, and death is imminent. During irreversible shock, cellular ATP is degraded into adenosine in the absence of oxygen as an electron receptor in the mitochondrial matrix. The Adenosine moves out of cellular membranes into extracellular fluid where it forms uric acid thus causing further acidosis and capillary vasodilation. The deficiency of intracellular adenosine prevents phosphorylation of ATP even after restoration of oxygen delivery in the cells in irreversible shock [4-6].
The four classifications of hypovolemic shock are depicted in (Table 1), and they are based on the percentage of volume of blood loss and the severity of the derangements in patient’s clinical parameters. Delays in reaching and receiving life-saving obstetric services by these critical ill patients are the major causes of the preventable obstetric catastrophes [7,8]. The treatments are not usually available in most rural communities and birth centers [9,10]. Where the hemorrhages usually occur. It often takes hours or even days for the ‘lucky ones’ to be alive until they access the life-saving services in the urban hospitals. Many of them often die at home or in transit to hospital. The NASG (Figure 2) is a first-aid-life-sustaining-device that can avert maternal deaths and shock-related morbidities during the delays [11,12]. It is a lower body suit of articulated neoprene and Velcro segments that provides rapidly lower body circumferential counter pressure of 20-40 mmHg that decreases the distal aortic mean baseline blood flow of 1.99 l/min by 0.65, and thus shunts blood flow from the lower limbs and the pelvis to the heart, brain, lungs and kidneys like during the compensatory stage of hypovolemic shock [13,14]. Studies in Egypt and Nigeria on obstetric hemorrhage confirmed that the NASG can reduce pelvic blood loss by 50%, prevent emergency hysterectomy, and shock-related morbidities like irreversible shock, multiple organ failures and maternal deaths [15-17]. The aims of this study are to reappraisal the effectiveness of NASG in averting maternal deaths and shock-related morbidities in severe obstetric hemorrhagic shock patients, and to make recommendations.
Settings and methods
Enugu State University Teaching Hospital (ESUTH) Enugu is a state owned health institution that evolved from Nursing Home in 1930 to a teaching hospital status in June 2006, and most of the population in the state are Christians and of the Igbo tribe [18,19]. The department of Obstetrics and Gynecology in ESUTH has two professors, a reader, 8 consultants, 9 senior registrars, 13 registers, house officers, and 45 staff nurse midwives. The obstetric unit has 42 beds, and 1250 deliveries occur annually. The department has labor ward and gynae emergency teams that operate 24 hours every day including Saturday and Sunday. Critical ill patients are referred to the department without restrictions. In 2016, three NASG were purchased by the department to be used in sustaining the lives of critical ill patients in shock that are referred to the hospital. Critical patients in severe hemorrhagic shock (stages 3 and 4) with any of these parameters were included in this reappraisal: systolic blood pressure <100 mmHg, mean arterial pressure <70 mmHg, pulse rate> 120 beats per minute, respiratory rate >30 breaths per minute, unconscious or altered mental status, and urine output of <20 ml/hour. Mild to moderate hemorrhagic shock patients and those who refuse NASG application were excluded. Immediately severe shock was diagnosed, the NASG was applied, and intravenous infusion of normal saline was started at a rate of 1.5 liters in the first one hour, and then maintained at 1liter every 8 hours till cross matched blood became available. The patient level of mental status, rate of bleeding, and vital signs were checked immediately after the application, and then reviewed at 15-30 minute intervals. Hourly urine output and intermittent oxygen saturation (where available) were also used to monitor patients on NASG. The NASG was removed in segments at 15-minute intervals with documentation of pulse rate and blood pressure immediately before and after removal of each segment (starting from the first segment). The criteria for the removal include the patient became conscious, the pulse rate and blood pressure were normal and stable for at least 2-6 hours, the mean arterial blood pressure was >70 mmHg and above, and bleeding stopped or reduced. The intravenous infusion was maintained running after removal of NASG. If the blood pressure falls by 20 mmHg or the pulse increases by 20 beats per minute (Rule of 20) at any point during the removal process or if there is an increase in vaginal bleeding; all the segments will be quickly replaced, and the patient reviewed to determine the sources of the bleeding. The main outcome measures were: restorations of the calculated mean arterial pressure to 70 mmHg and above, improvement on mental status, reduction on rate of bleeding, and prevention shockrelated morbidity and mortality. Time interval between application of NASG and the availability of cross matched blood and definite care were also noted.
Case 1
Mrs. DR was a 32-year-old Para 2+0 woman who had lower uterine segment scar rupture during vagina birth after a previous caesarean delivery at 41 weeks gestation that was assisted with vacuum extraction in a private hospital. A live male baby that weighed 3.6 kilograms with Apgar scores of 6 and 8 at first and fifth minutes respectively was delivered. She had severe vaginal bleeding that prompted her immediate transferred to ESUT Teaching hospital. On admission on 25/7/2016, Mrs. DR was conscious, but restless, and on blood transfusion from the referral private hospital. Her vital signs were: pulse rate of 120 beats per minute, blood pressure of 80/50 mmHg (calculated mean arterial blood pressure (MAP) of 60 mmHg) and respiratory rate of 44 cycles per minute. The NASG was applied, and another intra venous access was secured with a 16G cannula. The packed cell volume was 11%, and the bed side clotting time was 4 minutes. Three more units of fresh whole blood were cross matched. The parameter improved slightly on the application of the NASG. Her pulse rate became 110 beat per minute, blood pressure 90/50 mmHg, mean arterial pressure 63.3 mmHg, and respiratory rate 40 cycles per minute. The findings at exploratory laparotomy confirmed ruptured lower uterine segment scar, and 800 mls of hemo-peritoneum. The uterine tear was only repaired. She received a total of 7 units of blood. The postoperative recovery was satisfactory. The patient, husband, mother and father were counseled on the need for elective caesarean delivery in her subsequent pregnancies. She was discharged on the 8th postoperative day with a packed cell volume of 26%.
Case 2
Mrs. NC was a 35-year Para 3+0 woman who was admitted on 4/8/2016 at 12.40 pm on account of unscarred uterine ruptures that extended to the cervix, and severe primary postpartum hemorrhage that started after vaginal delivery of a live 2.9 kg female baby in a maternity home. She admitted that two white tablets (400 μg Misopristol) were administered to her sublingually during her labor management in addition to an ongoing oxytocin infusion. She was conscious on admission, but very pale and weak. The pulse rate was 110 beat per minute, blood pressure 90/50 mmHg (mean arterial pressure (MAP) of 63.3 mmHg), and respiratory rate 28 cycle per minute. NASG was applied, intravenous infusion of normal saline commenced, and the cervical laceration was repaired by the registrar. The cross matched blood became available after 1 hour 25 minutes. Even after 2 pints of blood transfusion, the bleeding continued, and vital signs continued to deteriorate. Pulse rate became 120 beat per minute, blood pressure 80/30 mmHg (MAP 46 mmHg), respiratory rate 26 cycle per minute, and SPO2 98% after about 4 hours of admission. Examination under anesthesia and exploratory laparotomy were done. Bleeding from uterine cavity and repaired posterior cervical laceration were noted. At exploratory laparotomy 1.5 liter of hemoperitoneum, and lateral uterine rupture extending to the cervix were noted and repaired with vircryl [2]. The bleeding stopped and the vital signs became stable. Seven hours after surgery her blood pressure was138/88 mmHg, MAP 104.7 mmHg, respiratory rate 28 breaths per minute, pulse rate 92beats per minute and SPO2 99%. She made 500 mls of clear urine. The NASG was removed. She had a total of 8 pints of blood transfused before she was discharged on the 7th postoperative day with packed cell volume of 25%.
Case 3
Mrs. AF was a 25-year Para 2+0 woman who delivered a 2.8 kg female fresh stillbirth in a health center, and had postpartum eclampsia, vaginal laceration and severe primary postpartum hemorrhage and shock. She was referred to ESUT Teaching Hospital on 28/8/16. She was admitted in an unconscious state with cold clammy extremities, and pitting pedal edema. She was pulseless, blood pressure could not be measured; but the heart sounds were present, urethral catheter drained 500mls of cokecolor urine on admission. The uterus was about 18 week size and contracted. Vaginal examination revealed anterior and post multiple vaginal lacerations. There was no cervical tear. NASG was applied before intra venous access could be secured with size 18 G cannula. Intra venous infusion of normal saline, 200mg hydrocortisone, and antibiotics were commenced. The bedside clotting time was 6 minutes. The lacerations were repaired under local anesthesia with vicryl size 1. The packed cell volume was 16%, and the urine protein was 2+. Within 30 minutes of the above interventions, and the pulse rate became 128 beat per minute, blood pressure 80/60 mmHg, mean arterial pressure 66.7 mmHg, and respiratory rate 48cycle per minute. Subsequent review after 3 hours, she had received 2 liters of normal saline and 1pint of whole blood transfused. The pulse rate became 100 beat per minute, blood pressure 120/80 mmHg, MAP 93.3 mmHg, and respiratory rate 32 cycle per minute. She made 400 ml of clear urine. She was still unconscious and the second pint of whole blood was commenced. The NASG was removed after 6 hours of stable vital signs. She became conscious next day, but her blood pressure rose to 170/130 mmHg. She was successfully managed with magnesium sulphate and oral antihypertensive drugs. She was discharged after 5 days of admission with blood pressure of 120/80 mmHg, and packed cell volume of 22%, oral antihypertensive drugs and hematinic. She was seen in the postnatal clinic two weeks later in good health with packed cell volume of 28% and blood pressure of 120/80 mmHg. She was referred back to the health center for further community follow up care.
Case 4
Mrs. UI was a 35-year Gravida 7 Para 6+0 woman with 4 living children who had an emergency caesarean delivery in a missionary hospital in 2012. She was admitted to our labor ward on 19/3/2017 at 2.00am on account of profuse recurrent painless vaginal bleeding of 2 days duration at 36 week gestation. She was unconscious, pulseless and the blood pressure could not be measured. NASG was then applied without the pelvic and abdominal segments before intra venous line with 18G cannula could be secured, and intra venous hydrocortisone 200 mg and 1.5 liter of normal saline given fast. Thirty minutes later the pulse rate became 134beat per minute, respiratory rate 34breath per minute, blood pressure 84/45 mmHg, and MAP 58 mmHg. She was taken to theater for exploratory laparotomy with one pint of cross matched blood running. Massive hemo-peritoneum >3 liters, 3.1 kg female fresh stillbirth and extensive lower segment scar rupture extending to the left broad ligament were found at surgery. She had subtotal hysterectomy, and 3 units of whole blood transfused intra operatively. The abdominal segment of the NASG was then applied after the surgery. Immediate postoperative vital signs were pulse rate 130 beat per minute, respiratory rate 28 breath per minute, and blood pressure 110/70 mmHg. She had 6 pints of blood transfused and was discharged on the 13th postoperative day with packed cell volume of 29%.
Discussion
Severe hemorrhagic shock is a ‘killer disease’ especially when there are delays in reaching and/or receiving appropriate emergency obstetric care. Early recognition of hemorrhagic shock is essential to the successful management. Hemorrhage, tachycardia, high respiratory rate, restlessness, coma, hypotension, low mean arterial pressure, narrow pulse pressure, and reduced urine output are common findings in hemorrhagic shock. The principles of management of severe hemorrhagic shock are: keep the patient alive, avoid further harm, and quickly transfer the patient to hospital for urgent identification of the sources of bleeding, blood transfusion and definitive rescue surgery. The patient can be kept alive by calling for helps to assist you in applying NASG, securing wide bore intravenous line with 16G cannula and starting crystalloid infusion, organizing ambulance or transport for safe transfer of patient to hospital, and writing the referral note. Ensure patient’s airway is patent and give oxygen. Several studies including this work have confirmed the effectiveness of the NASG as a first-aid-lifesustaining- device that can sustain the lives of critical ill shock patients until cross matched blood and definitive interventions become available [12-17]. The normal saline infusion was limited to 1.5 liter instead of the usual recommendation of 3:1 to avoid fluid overload as the vascular volume is restricted by the NASG application. The patients in this study were admitted in critical states. Cases 3 and 4 were unconscious, pulseless and the blood pressure could not be measured. The applications of NASG restored the pulses and the blood pressures. More importantly, the veins of the patients become visible for securing intravenous access. The establishment of intravenous access or ‘life-line’ is a very important role of NASG in the resuscitation of patients in shock. The administration of steroids, crystalloid infusions, blood transfusion and other medications are possible if there is intravenous access. However, in case 2 the vital signs continued to deteriorate in spite of the application of NASG because the sources of the bleeding were not completely identified. The registrar only sutured the cervical laceration but the vital signs became stable as soon as the uterine rupture was also repaired. It is very important to understand that the NASG is a lifesustaining- device, and not the treatment of shock. There were improvements on the mental status, vital signs including the calculated mean arterial pressure (MAP) in all the patients as soon the garments were applied. These parameters became normal and stable after adequate blood transfusions and definitive surgeries were done. MAP=(Systolic blood pressure +2 × Systolic blood pressure) ÷ 3. It is an index of oxygen tissue perfusion (normal range is 65-110 mmHg). MAP that is greater than 70 mmHg can sustain the oxygen perfusion of the organs, and prevent further harms like irreversible shock, renal failure, coagulopathy, multiple organ dysfunction and death as in my patients. Other parameters for monitoring the effectiveness of NASG include urine output ≥ 30 ml/hour, respiratory rate <20 breaths per minute, reduced bleeding and clearance of sensorium. Seventy five percent of the patients in this series remained conscious when on NASG. The prolonged unconscious state in case 3 may be due to the severe postpartum eclampsia.
Uterine scar rupture accounted for 50% of the severe shock in this study. Policies must be made to ensure that such high risk labors occur in equipped hospitals with adequate manpower and blood to avoid preventable calamities. A total of 25 pints of blood were used by the 4 patients. The NASG was able to prevent shock-related morbidity and mortality in the patients.
Recommendations
NASG should be available in every childbirth center as hemorrhagic shock can be an unpredictable dire emergency. Skilled birth attendants should be trained on the use of the NASG and regular drills or stimulations practiced to maintain efficiency. Patients on NASG need only basic monitoring devices.
Conclusion
NASG is effective in resuscitating and sustaining women in severe obstetric hemorrhagic shock. The causes of the shock must be identified and properly treated to optimize its effectiveness. There was neither mortality nor clinically significant morbidity in this reappraisal. Patient must closely be assessed immediately after application to detect signs and symptoms of undiagnosed heart disease. NASG is cheap, and has safety features for wider utilization. It is of immense benefit in settings where there are delays in initiating treatment for severe hemorrhagic shock (Table 2).
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Age in years | 32 years | 35 years | 25 years | 35 years |
| Admission date | 25/7/2016 | 4/8/2016 | 28/8/2016 | 19/3/2017 at 36 weeks |
| Parity | Para 2+0, 1 prev CD | Para3+0 | Para 2+0 | G7Para 6+0 1prev CD |
| 2 Males | ||||
| Number of living children | 2 females, 1 male | 1 male stillbirth | 3female 1male alive | |
| None alive | ||||
| Causes of shock | Uterine scar rupture in vacuum assisted vaginal birth after a prev CD at 41 weeks | Unscarred uterine rupture that extended to the cervix. 400 µg misopristol used sublingually in labor | Multiple vaginal lacerations and primary postpartum hemorrhage | Uterine scar rupture in attempted vaginal birth after a prev CD |
| Patient parameters on admission: | ||||
| Mental status | Conscious, restless | Conscious | Unconscious | Unconscious, |
| Pulse rate | 120 | 110 | Pulseless | Pulseless |
| Resp rate (bpm) | 44 | 28 | NS | NS |
| BP (mmHg) | 80/50 | 90/50 | Not measurable | Not measureable |
| MAP (mmHg) | 60 | 63.3 | - | - |
| Packed cell volume | 11% | NS | 16% | NS |
| Urine output/ hour | NS | NS | NS, Proteinuria 2+ | NS |
| Parameters after NASG application: | Conscious | *Bleeding continued after suturing of cervical tear | *iv access secured | *iv access secured |
| Mental status | Conscious | 120 | Unconscious? eclampsia | Conscious |
| Pulse rate (bpm) | 128 | |||
| 110 | 46 | 134 | ||
| Resp. rate (bpm) | 48 | |||
| BP (mmHg) | 40 | 80/30 | 80/60 | 34 |
| 90/50 | 46 | 84/45 | ||
| MAP (mmHg) | 63.3 | ---- | 66.7 | 58 |
| Packed cell volume | ----- | NS | 16% | ---- |
| Urine output / hour | 133 ml/hour | |||
| NS | NS | |||
| Number of pints of blood transfused | 7 | 8 | 2 | 6 |
| Definite treatment or surgery | Uterine repair only | Uterine and cervical repairs | Suturing of multiple vaginal lacerations | Subtotal hysterectomy. |
| 800 mls of hemoperitoneum | 1.5 liter of hemoperitoneum | >3 liters of hemoperitoneum | ||
| Prevention of shocked-related morbidity and mortality | Prevented | Prevented | Prevented | Prevented |
Definitions: NASG: Non-pneumonic Anti-Shock Garment, Prev CD: Previous Caesarean Delivery, G7: Gravida 7, NS: Not Stated, BP: Blood Pressure, MAP: Mean Arterial Pressure.
Table 2: Summary of the cases and their responses to NASG application.
Dedication
This work is dedicated to my mentor and professional father, Nweke, for being my Non-Pneumatic Anti-Shock Garment (NASG) that sustained my life during my difficult residency training in Obstetrics and Gynecology. You made me to believe in myself and to promise you that ‘I will never abandon’ the training. Sir, I will ever remain grateful to you all the days of my life.
References
- WHO (2013) Postpartum haemorrhage. Priority diseases and reasons for inclusion 6: 16.
- WHO (2000) Managing Complications in Pregnancy and Childbirth: A guide for midwives and doctors. Integrated Management of Pregnancy and Childbirth (IMPAC) Geneva: WHO, Department of Reproductive Health and Research 22.
- Kumar F, Vinay S, Abbas E, Abul K, Fausto K (2010) Robbins Basic Pathology. Saunders Elsevier 2: 102-103.
- Guyton E, Arthur H, John D (2012) Circulatory Shock and Physiology of Its Treatment". In Gruliow, Rebecca. Philadelphia, Pennsylvania: Elsevier Inc 22: 278-288.
- Hudson K, Kristi W (2004) "Hypovolemic Shock - 1 Nursing CE". Archived from the original on 6: 26.
- Elizabeth D, Agabegi F, Agabegi SS (2012) Step-Up to Medicine (Step-Up Series). ISBN 12: 7146-7153
- Thaddeus S, Maine D (2009) Too far to walk: maternal mortality in context. Soc Sci Med 38: 1091-1110.
- Doumouchtsis SK,Arulkumaran S (2004) Postpartum haemorrhage: changing practices. In: Ledger W, Dunlop W (editors). Recent advances in obstetrics & gynaecology . London, UK: Royal Society of Medicine Press Ltd
- Nkwo PO, Lawani LO, Ubesie AC, Onodugo VA, Obu HA, et al. (2008) Poor availability of skilled birth attendants in Nigeria: A case study of Enugu state primary health care system. Ann Med Health Sci Res 5: 20-25.
- II Okafor EO, Ugwu EO, Ndibuagu R (2013) Amenities that can Attract Skilled Birth Attendants to Practice in Rural Areas of a Developing countries. World J. Clin. Pharmacol. Microbiol. Toxicol 4: 30-37.
- Lalonde A, Daviss BA, Acosta A (2010) Postpartum hemorrhage today: ICM/FIGO initiative. Int J Gynaecol Obstet 94: 243-253.
- Tsu VD (2009) New and underused technologies to reduce maternal mortality. Lancet 363: 75-76.
- Miller S, Ojengbede A, Turan JM (2009) Anti-shock garments for obstetric hemorrhage. Current Women’s Health Reviews 3: 3-11.
- Hauswald M, Michael R, Williamson E, Gillian M, Baty, et al. (2005) Victoria LEdgar-Mied. Use of an improvised pneumatic anti-shock garment and a non-pneumatic anti-shock garment to control pelvic blood flow Int J Emerg Med 3: 173-175.
- Miller S, Hamza S, Bray E (2004) First aid for obstetrical hemorrhage: the pilot study of the Non-Pneumatic Anti-Shock Garment (NASG) in Egypt. Int J Emerg Med 113: 424-429.
- Miller S, Turan J, Dau K (2005) Use of the Non-Pneumataic Anti-Shock Garment (NASG) to reduce blood loss and time to recovery from shock for women with obstetric hemorrhage in Egypt. Glob Pub Health 2: 110-124.
- Mourad-Youssif M, Oladosu AO (2013) Carinne D Meyer, Mohammad Fathalla, Imran O Morhason-Bello.Can the Non-pneumatic Anti-Shock Garment (NASG) reduce adverse maternal outcomes from postpartum hemorrhage? Evidence from Egypt and Nigeria. Reproductive Health 7: 24
- Okafor II, Ugwu EO, Obi SN, Odugu BU (2007) Virtual elimination of motherto-child transmission of human immunodeficiency virus in mothers on highly active antiretroviral therapy in Enugu, South-Eastern Nigeria. Ann Med Health Sci Res 4: 615-618.
- Dim CC1, Ugwu EO, Iloghalu EI (2012) Duration and determinants of interbirth interval among women in Enugu, south-eastern Nigeria. J Obstet Gynaecol 33: 175-179
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences