Couvelaire Uterus
Maria Hijji
Department of Gynecology, Mohammed V University, Rabat, Morocco
Published Date: 2023-06-30Maria Hijji*
Department of Gynecology, Mohammed V University, Rabat, Morocco
- *Corresponding Author:
- Maria Hijji
Department of Gynecology,
Mohammed V University,
Rabat,
Morocco;
Email: mariahijji91@gmail.com
Received: September 29, 2023, Manuscript No. IPCCO-23-15434; Editor assigned: October 03, 2023, PreQC No. IPCCO-23-15434 (PQ); Reviewed: October 17, 2023, QC No. IPCCO-23-15434; Revised: October 24, 2023, Manuscript No. IPCCO-23-15434 (R; Published: October 30, 2023,DOI: 10.36648/2471-9803.9.5.135
Citation: Hijji M (2023) Couvelaire Uterus. Crit Care Obst Gyne Vol.9 No.5:135.
Abstract
Couvelaire uterus is a phenomenon where the retroplacental blood may penetrate through the thickness of the wall of the uterus into the peritoneal cavity. This may occur after abruptio placentae. The hemorrhage that gets into the decidua basalis ultimately splits the decidua and the haematoma may remain within the decidua or may extravasate into the myometrium). The myometrium becomes weakened and may rupture due to the increase in intrauterine pressure associated with uterine contractions. This may lead to a life-threatening obstetric emergency requiring urgent delivery of the fetus. The uterus should be evacuated and contractions should be stimulated using intravenous oxytocin; hysterectomy (the removal of the uterus) may be needed in some cases.
Keywords
Retroplacental haematoma; Uterine apoplexy; Couvelaire; Myometrium
Introduction
Early in the 20th century, French doctor Alexandre Couvelaire coined the term uteroplacental apoplexy to characterise it [1]. Because it has historically only been detected through direct intraoperative visualisation, its incidence is difficult to assess. Radiologic correlation with operative results has not previously been recorded because imaging is typically contraindicated in this clinical scenario. Couvelaire uterus is caused when haemorrhage from placental blood vessels seeps into decidua basalis causing placental separation, followed by infiltration in the lateral portions of the uterus [2]. Occasionally, the infiltrations reach the peritoneal cavity. Couvelaire uterus is managed conservatively.
Couvelaire uterus is a phenomenon where the retroplacental blood may penetrate through the thickness of the wall of the uterus into the peritoneal cavity [3]. This may occur after abruptio placentae [4]. The hemorrhage that gets into the decidua basalis ultimately splits the decidua and the haematoma may remain within the decidua or may extravasate into the myometrium (the muscular wall of the uterus) [5]. The myometrium becomes weakened and may rupture due to the increase in intrauterine pressure associated with uterine contractions. This may lead to a life-threatening obstetric emergency requiring urgent delivery of the fetus. Only direct visualisation through a caesarean section or a biopsy (or both) can diagnose this syndrome. This is why the literature under reports and underestimates its occurrence.
The capacity of a couvelaire uterus to contract is unaffected and decompression frequently enables constriction of spiral arteries to achieve hemostasis. In the event that appropriate hemostasis cannot be obtained due to diffuse intravascular coagulopathy, a hysterectomy may be advised as a life-saving procedure [6]. Our case emphasises the significance of prompt surgical intervention with emergency hysterotomy for life-saving measures in a clinically unstable pregnant female with suspected abruption. The ability of a couvelaire uterus to contract is unaffected and decompression frequently enables constriction of spiral arteries to achieve hemostasis [7]. When disseminated intravascular coagulopathy prevents hemostasis from being established satisfactorily, a hysterectomy may be recommended as a life-saving procedure.
The occurrence of couvelaire uterus can be prevented by prevention of abruptio placentae. This includes proper management of hypertensive states of pregnancy; treatment of maternal diseases like diabetes mellitus and other collagen disease complicating pregnancy; prevention of trauma during pregnancy; mothers should also avoid smoking or consumption of alcohol during pregnancy [8]. The uterus should be evacuated and contractions should be stimulated using intravenous oxytocin; hysterectomy (the removal of the uterus) may be needed in some cases. The foetus may be compromised if there is prolonged delivery because of the non-contractile uterus; severe bleeding may cause hypovolemic shock in the mother.
Symptoms
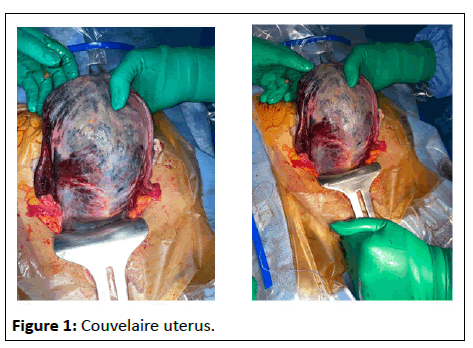
Patients may have localised uterine discomfort, uterine tetany or pain owing to uterine contractions. Foetal distress, foetal death and abruptio placentae signs can also manifest as uterine hypertonus, foetal distress and in rare cases, hypovolemic shock (shock brought on by significant blood loss). The extravasation of blood into uterine muscle may cause the uterus to take on a bluish/purplish, mottled appearance.
Case Presentation
We here report the case of a 40 years old, with a personal history of chronic hypertension under aldomet, without any surgical history.
• G1: Spontaneous miscarriage at 1 month, uncured at home undetermined context.
• G2: Spontaneous miscarriage at 2 month, uncured at home undetermined context.
• G3: Spontaneous miscarriage at 2 months, uncured at home undetermined context.
• G4: Current pregnancy estimated at 5 months according to DDR inaccurate, pregnancy poorly monitored and no prenatal check-up done.
According to an obstetrical ultrasound of 21 SA made on 24/05/2022, this current pregnancy is at 25 SA. On admission, patient with a GCS: 15/15. BP 17/11, no positive headaches, no ringing in the ears, no visual fog, proteinuria at labstix at 1 cross. Obstetrical ultrasound: Monofetal pregnancy not evolving, measurements of 24-25 SA. Vaginal examination: Open cervix with expulsion of the fetus, with moderate bleeding.
Expulsion of a macerated male fetus PN: 800 g. Directed delivery with uterine revision done bringing back blackish clots, (10 IU of syntocinon IM+2 g of Maxiclav IVD) were administered the patient presented a post abortal hemorrhage, agitated patient, resuscitator on duty on site, decision to take charge of the patient in the operating theatre.
Implementation of the hemorrhage protocol: 40 IU of syntocinon/1 g exacyl, under-valve examination: Purplish blue cervix with no cervical or vaginal lesions, abundant red endouterine bleeding, absence of the safety globe, packing for 20 minutes. Re-evaluation of bleeding; active red, abundant endouterine, absence of the uterine globe, decision of laparotomy for delivery hemorrhage/uterine inertia. Surgical report: Pfann type incision, plane opening by paln. Exploration: Atonic and friable apoplectic uterus of couvelaire.
A triple ligature was performed, but this did not stop the bleeding. Subtotal inter-annexal haemostasis hysterectomy, hemostasis assured, plane by plane closure. Transfusion of 5CG intraoperatively. Immediate postoperative follow-up: Patient intubated under anuric noradrenaline BP: 9/6 HR: 123 Bpm. Patient J1 postoperative, extubated, conscious BP: 16/10 HR: 87 bpm. Put on loxen at SAP+loxen 50 mg orally, diuresis restarted, bleeding: negative (Figure 1).
Results and Discussion
Couvelaire uterus is a rare manifestation to find in a previable pregnancy. The incidence of couvelaire uterus is difficult to estimate since the diagnosis can only be reached intraoperatively. In most cases it occurs with abruption placentae which develops due to a disruption in the vessels within the placenta allowing for blood to seep into the decidua basalis leading to premature separation of the placenta and bleeding into the myometrium which may extend to the parametrium and peritoneum [9-11]. Clinicians should be vigilant when dealing with vaginal bleeding in a pre-viable pregnancy and placental separation is considered as an important differential to avoid the maternal morbidity and mortality that may ensue.
Couvelaire uterus, also previously known as uteroplacental apoplexy. First described in the medical literature by Dr. Alexandre Couvelaire, a French obstetrician in 1912. This is a lifethreatening condition resulting from bleeding into the myometrium that may extend to the parametrium and peritoneum [12,13]. Couvelaire uterus is typically associated with abruptio placentae, the premature separation of the placenta. This condition is usually diagnosed by direct visualization of the uterus during caesarean section [14]. For this reason, its prevalence is perhaps underreported and underestimated in the literature.
Couvelaire uterus is a potentially fatal severe form of placental abruption. This is a significant cause of antepartum haemorrhage that is commonly associated with maternal and neonatal morbidity and mortality [15].
Conclusion
We present a rare case series of couvelaire uterus in previable pregnancy in Aga Khan hospital, Dares salaam. This combination is a rare occurrence and there are no cases reported in sub- Saharan Africa from our literature search using various search engines. This paper has been reported in line with the SCARE 2020 criteria. This article has been registered with the research registry with identification number research registry 8362 and can be found through the following hyperlink browse the registry-research registry.
References
- Hubbard JL, Hosmer S (1997) Couvelaire uterus. J Osteopath Med 97: 536.
[Crossref] [Google Scholar] [PubMed]
- Donaldson IA, Bismillah AH (1963) Life from a couvelaire uterus. Postgrad Med J 39: 356.
[Crossref] [Google Scholar] [PubMed]
- Lee YJ, Calvert K, Jape K (2022) Couvelaire uterus resulting in haemoperitoneum. J Surg Case Rep 2022: 618.
[Crosserf] [Google Scholar] [PubMed]
- Uwagbai ON, Wittich AC (2017) A 30-year-old female found to have a couvelaire uterus with placenta accreta during planned cesarean delivery. Mil Med 182: e1877-e1879.
[Crossref] [Google Scholar] [PubMed]
- Ming GS, Lee WK, Tan SQ (2020) An unusual case of placenta abruption leading to couvelaire uterus in a previable pregnancy. J Med Cases 11: 103.
[Crossref] [Google Scholar] [PubMed]
- Beischer NA (1966) Traumatic rupture of a couvelaire uterus. A N Z J Surg 35: 255-258.
[Crossref] [Google Scholar] [PubMed]
- Khalifa AA, MA E, Ahmed MM, Elshamandy MM (2021) Huge post-partum intra-myometrial hematoma (couvelaire uterus) in a preserved uterus in a case of placenta accreta: Case report. Egypt J Hosp Med 84: 2173-2175.
- Tskhai VB, Levanova EA (2021) The possibility of using organ-sparing tactics in patients with a couvelaire uterus. Obstet Gynecol 200-205.
- Kapesi V, Moshi B, Kyejo W, Jusabani A, Mgonja M, et al. (2023) Couvelaire uterus in a previable pregnancy: Complication in abruptio placenta, case series from Tanzanian tertiary hospital. Int J Surg Case Rep 102: 107862.
[Crossref] [Google Scholar] [PubMed]
- Vijayashree M (2016) A clinical study of maternal and fetal outcome in abruptio placenta-couvelaire uterus a preventable obstetric catastrophe. Sri Lanka J Obstet Gynaecol 37.
- AbdRabbo SA (1994) Stepwise uterine devascularization: A novel technique for management of uncontrollable postpartum hemorrhage with preservation of the uterus. Am J Obstetr Gynecol 171: 694-700.
- Kehila M, Hmid RB (2016) Couvelaire uterus: Bad aspect but normal uterine function. Pan Afr Med J 25: 11.
[Crossref] [Google Scholar] [PubMed]
- Barclay DL (1970) Cesarean hysterectomy. Thirty years'experience. Obstet Gynecol Surv 25: 566-568.
[Google Scholar] [PubMed]
- Gogola J, Hankins GD (1998) Amniotic fluid embolism in progress: A management dilemma!. Am J Perinatol 15: 491-493.
[Crossref] [Google Scholar] [PubMed]
- Dashraath P, Wong YC (2020) Couvelaire Uterus. N Engl J Med 383: 1973.
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences