Androgens in Polycystic Ovarian Syndrome (PCOS) Beyond Testosterone.
Prem Narayanan
Prem Narayanan*
Department of Endocrinology and Metabolism, Amrita Institute of Medical Sciences, Kochi, India
- *Corresponding Author:
- Prem Narayanan
Department of Endocrinology and Metabolism
Amrita Institute of Medical Sciences, Kochi, India
Tel: 03920313687
E-mail: premnarayanan@aims.amrita.edu
Received date: June 13, 2020; Accepted date: July 31, 2020; Published date: August 7, 2020
Citation: Narayanan P (2020) Androgens in Polycystic Ovarian Syndrome (PCOS) Beyond Testosterone. Crit Care Obst Gyne Vol.6 No.3:6.
Abstract
PCOS (Reproductive Metabolic Syndrome) is the most common endocrine disorder in women of reproductive age group (5-15%). One of the major criteria for diagnosis is clinical or biochemical (Total testosterone >55ng/dl or free testosterone 9pg/ml) hyperandrogenism. There has always been a disparity between FG score and Testosterone (T) levels in PCOS women. Around half of those with mild hirsutism and small proportion of those with moderate-severe hirsutism are not associated with biochemical hyperandrogenism.
Commentary
PCOS ( Polycystic Ovarian Syndrome ) is the most common endocrine disorder in women of reproductive age group (5%-15%). One of the major criteria for diagnosis is clinical or biochemical (Total testosterone>55 ng/dl or free testosterone 9 pg/ml) hyperandrogenism. There has always been a disparity between FG score and Testosterone (T) levels in PCOS women. Around half of those with mild hirsutism and small proportion of those with moderate-severe hirsutism are not associated with biochemical hyperandrogenism. The circulating levels of testosterone vary according to the diurnal rhythm, phase of menstrual cycle, SHBG, time of day and reproductive maturity. The commercially available immunoassays are not standardized for female range (20 ng/dl-60 ng/dl) on which to base an assay. The gold standard is LC-MS but it costly and time consuming hence limited to research purposes. Some studies showed calculated free testosterone and free androgen index as better screening tool for hyperandrogenemia than total testosterone.
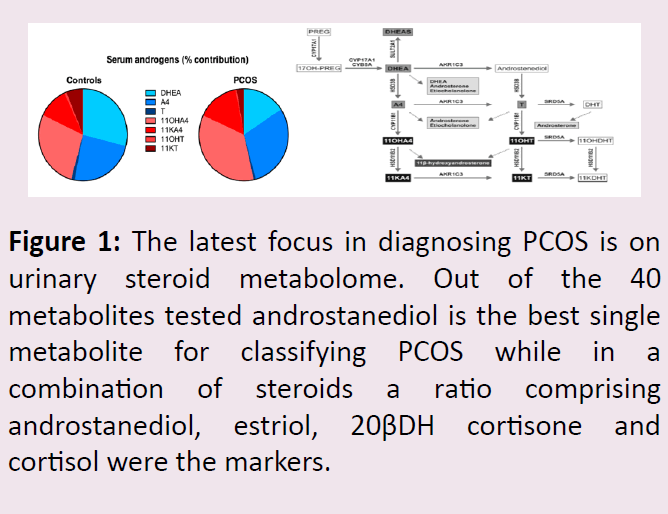
Functional adrenal hyperandrogenism is also pathogenic feature of PCOS and testosterone precursor Androstenedione (A4) shown to be a more sensitive marker of PCOS-related androgen excess and, in combination with T, predictive of metabolic risk. It has also been shown that androstenidione–free testosterone ratio have a favorable metabolic profile. DHEA-S is mainly used to rule out adrenal cause for hyperandrogenism rather than as a marker for PCOS. The recent focus has been on 11-oxygenated C-19 steroids in PCOS. 11OHA4 is a major product of adrenal steroidogenesis and its downstream conversion to 11-ketotestosterone (11KT) and 11-keto-5a-dihydrotestosterone which can bind and activate the androgen receptor with affinities and potencies similar to that of T and 5a-dihydrotestosterone, respectively. 11-KT has been shown to be 3-fold higher than T in PCOS (Figure 1).
Figure 1: The latest focus in diagnosing PCOS is on urinary steroid metabolome. Out of the 40 metabolites tested androstanediol is the best single metabolite for classifying PCOS while in a combination of steroids a ratio comprising androstanediol, estriol, 20βDH cortisone and cortisol were the markers.
References
- Stanczyk FZ, Lee JS, Santen RJ (2007) Standardization of steroid hormone assays: why, how, and when? Cancer Epidemiol Biomarkers Prev 16: 1713-1719.
- Lerchbaum E, Schwetz V, Rabe T, Giuliani A, Obermayer-Pietsch B (2014) Hyperandrogenemia in polycystic ovary syndrome: exploration of the role of free testosterone and androstenedione in metabolic phenotype. PLoS One 9: e108263.
- O’Reilly MW, Kempegowda P, Jenkinson C, Taylor AE, Quanson JL, et al. (2017) 11-Oxygenated C19 steroids are the predominant androgens in polycystic ovary syndrome. J Clin Endocrinol Metab 102: 840-848.
- Dhayat NA, Marti N, Kollmann Z, Troendle A, Bally L, et al. (2018) Urinary steroid profiling in women hints at a diagnostic signature of the polycystic ovary syndrome: A pilot study considering neglected steroid metabolites. PloS One 13: e0203903.
- Rosenfield RL, Ehrmann DA (2016) The pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev 37: 467-520.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences