Seventeen Week Uterine Rupture: A Case Report
Tiffany R Tonismae, Christinne Canela and Elizabeth McCuin
DOI10.21767/2471-9803.100027
Tiffany R Tonismae*, Christinne Canela and Elizabeth McCuin
Obstetrics and Gynecology, Virginia Tech Carilion School of Medicine, USA
- *Corresponding Author:
- Tiffany R Tonismae
Ob/Gyn Resident, Obstetrics and Gynecology
Virginia Tech Carilion School of Medicine
1906 Bellview Ave, USA
Tel: 8035300493
E-mail: onismae@gmail.com
Received date: May 02, 2016; Accepted date: June 30, 2016; Published date: July 07, 2016
Citation: Tonismae TR, Canela C, McCuin E. Seventeen Week Uterine Rupture: A Case Report. Crit Care Obst&Gyne. 2016, 2:4. doi: 10.21767/2471-9803.100027
Copyright: © 2016 Tonismae TR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Uterine rupture occurs when there is complete or partial separation of the uterine wall. It is associated with increased morbidity and mortality for both the mother and the infant.
Case: A pregnant woman presents to the emergency room complaining of two weeks of abdominal pain at 17 weeks gestation. She was evaluated in an outlying emergency department when she became unstable and was transferred to a tertiary care center. A bedside ultrasound as well as commuted tomography revealed an extrauterine fetus, and she was taken to the operating room for exploratory laparotomy. Surgery revealed complete uterine rupture at the fundus with the fetus expelled into the abdomen.
Conclusion: This case offers review of a rare outcome of uterine rupture during the second trimester and risks factors to be monitored for futures cases.
Keywords
Uterine rupture; Second trimester; Hysterotomy scar
Introduction
Uterine rupture is classified as complete or partial separation of the uterine walls and is often associated with high morbidity and mortality [1]. There are several risks factors for uterine rupture with the most common being separation of a previous hysterotomscar. Other risks factors include trauma, injury, prior myomectomy or other uterine surgeries, or uterine anomalies [2]. Spontaneous rupture comprises a few as 1 in 15,000 deliveries [3].
Uterine rupture in the second trimester is very rare, especially without predisposing risk factors. While uterine rupture in a patient with a prior cesarean section often occurs at the site of the prior hysterotomy scar, a case of a patient with rupture in a location unrelated to her scar is noteworthy for the literature. This is a case of a patient with a history of two prior low transverse cesarean sections who presented with a fundal uterine rupture at seventeen weeks gestational age leading to fetal demise.
Case Report
A 32-year-old gravida 5, para 2 at 17 weeks and 1 day gestation presents to the emergency department complaining of mild abdominal pain, primarily located in the right upper quadrant, for the past month. She has previously been evaluated by both her primary obstetrician and in the emergency department of her local hospital. That morning, she had new onset vaginal bleeding with increasing abdominal discomfort, worse than previously. She was noted to be anemic with a hematocrit of 23 and subsequently became hypotensive, tachycardic, and diaphoretic while in the emergency department.
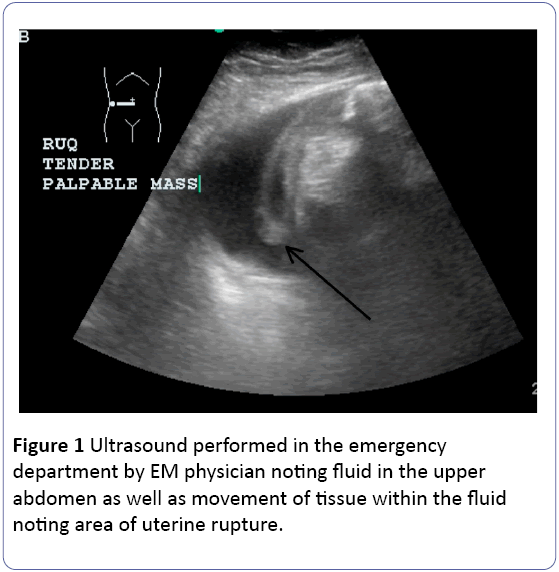
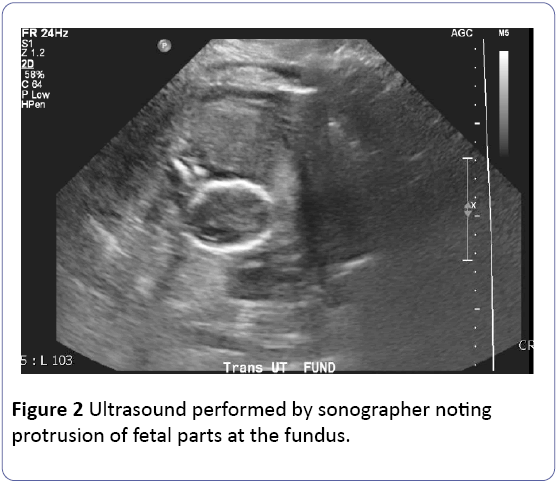
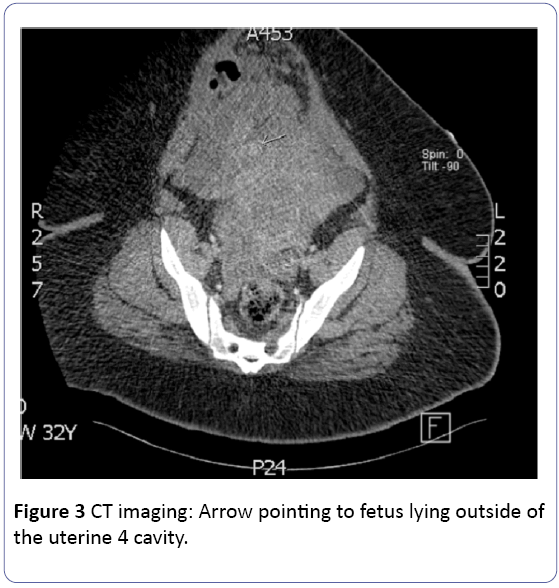
She was transferred to a higher-level facility at this time. Upon arrival, a limited transabdominal exam was obtained at the bedside by an emergency department resident noting a nonviable, extrauterine fetus. Of note, the infant measured approximately 16 days smaller than expected based on EDC from early imaging. Computed tomography was obtained by the emergency department to assess suspected uterine rupture noting similar findings with a fetus lying anterior to the uterine fundus and moderate hemoperitoneum (Figure 1). At this time, the obstetrics team was called for an emergency consult.
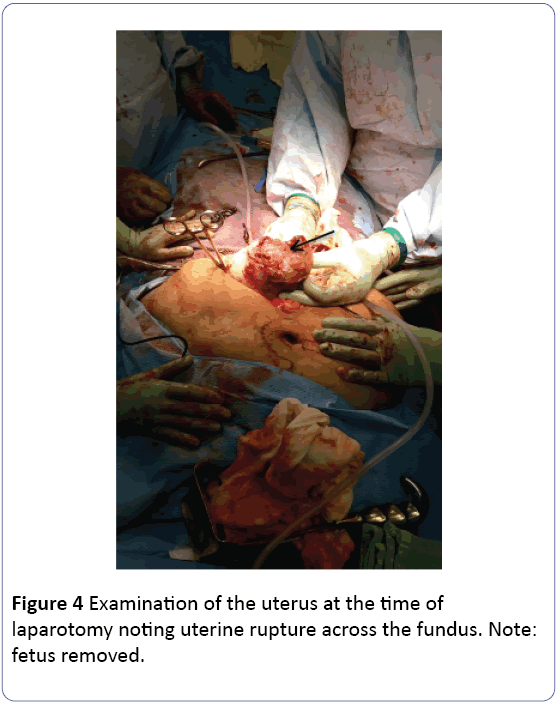
Transfusion protocol was started in the emergency department and the patient was taken immediately for an exploratory laparotomy. A vertical midline incision was made, and upon entrance into the peritoneum, significant amount of blood and clot was noted. The uterus was exteriorized from the abdomen noting full thickness transverse uterine rupture across the fundus measuring approximately five centimeters that did not extend to either fallopian tube. The fetus was completely extruded from the uterus with minimal placental attachment. Two to three liters of blood and clot were removed from her abdomen. There was no disruption of the prior cesarean hysterotomy site. There was an area on the small bowel that was concerning given its appearance (Figure 2). General surgery was consulted intra-operatively and they performed a smallbowel resection and re-anastomosis. Final pathology was 1 consistent with a four centimeter resolving hematoma. Due to significant bleeding and hemoperitoneum, a supracervical hysterectomy was performed. Normal adnexa were seen.
Prior to events leading to the aforementioned presentation, the patient had an uncomplicated pregnancy. She had regular obstetric care and a twelve-week ultrasound without noted uterine or placental anomalies. She had no reported history of abdominal trauma, drug use, smoking, or elevated blood pressures. She was on no medications other than prenatal vitamins. Her surgical history was significant only for two prior low transverse cesarean sections.
Discussion
Second trimester uterine rupture is exceedingly rare. The previous patient represents a case of a patient that would have an increased risk of uterine rupture at term at the point of prior hysterotomy, but without risks factors for rupture at an alternative location or in the second trimester. Uterine rupture can be fatal to the infant and can represent significant maternal morbidity and mortality, especially if it goes unrecognized. The risks of uterine rupture following one cesarean section is 0.7-0.9% while following two cesarean sections rises to 0.9-1.8% [4]. These risks, however, only represent rupture at the prior hysterotomy incision. In patients with second trimester demise undergoing medical management with prostaglandins, the risk of uterine rupture is estimated to be at 0.4% in women with one prior low transverse cesarean section according to a study by Berghella, et al.
In the same study, they did not see any cases of uterine rupture in the 46 women who had two prior low transverse cesarean sections (Figure 3). The risk of uterine rupture increased to 50% in this study in those who have had a prior classical cesarean delivery [5].
Cases have been reviewed for uterine rupture in patients without history of prior uterine incisions. In a review by Sun et al., fifteen cases of rupture were reviewed. Of these cases, 7 of these cases occurred in the second trimester with the uterine location within the fundus or cornua for most. Most of these cases also had presenting risk factors including uterine anomalies, abnormal placentation, or drug use [6]. While our patient did not present with these risk factors, there may be more information to be gained on review of these cases in that these rupture were also fundal location when they occur in the second trimester.
Early uterine ruptures have been noted in patients 1 with muellerian anomalies. These ruptures are often seen in patients with no history of uterine surgical procedures [7]. Abnormal placentation has also been noted as a cause for rupture in an unscarred uterus, most notably with placenta increta or percreta (Figure 4). Of cases reviewed with uterine rupture in an unscarred uterus available through the literature, the rupture site is most often located at the fundus or the cornua [8]. In laboring patients, the rupture site is often within the lower uterine segment that is thinned and the weakest site of the uterus. While second trimester uterine ruptures have been noted on rare cases, the rupture site most often occurs at the site of prior incision following several prior cesareans or may be related to trauma.
Signs of early uterine rupture may be harder to distinguish due to nonspecific symptoms. While many women present to the providers in the second trimester with vague complaints of non-specific abdominal pain, uterine rupture is not often high on the list of differentials. In this case, the patient had several weeks of abdominal pain before she became unstable and rupture was diagnosed. Many of the patient’s complaints were previously dismissed as “pains of pregnancy” in both the emergency department and obstetric office visit. It was not until the patient became unstable with vaginal bleeding that further investigation was performed. While not all patients with abdominal pain require extensive work-up, this case offers teaching opportunities to increase the differential diagnosis for persistent abdominal pain in the pregnant setting.
Conclusion
While second trimester uterine rupture may not present with the same magnitude of signs and symptoms seen closer to term, physicians need to consider the diagnosis in pregnant patients presenting with abdominal pain. Based on the estimated size of the fetus on ultrasound upon arrival in the emergency department and the prolonged symptoms, there is concern for the timing of the uterine rupture. While the patient had an acute change in hemodynamic stability during the current presentation, there is a possibility that the rupture had been present for many days or even weeks prior.
While the ultimate cause of rupture still remains unclear in this patient, our suspicion leans towards corneal placentation based on the location of the uterine rupture at the time of laparotomy. Similar to abnormalities seen with placental accreta, corneal placentations can cause a change in the integrity of the myometrium, increasing the risk of uterine rupture. While it may be possible that the rupture may have started off as a small defect, the outcome would most likely be unchanged. While some cases have looked at the possibility of repair of small defects, these have primarily been seen in rupture on the unscarred uterus. More cases would need to be reviewed to determine the plausibility of these procedures on rupture occurring on those patients with prior hysterotomy.
References
- Gary CF (2005) Prior Cesarean Delivery: Uterine Rupture, Williams Obstetrics. (23rdedn), McGraw-Hill Professional, New York.
- John QT, Spong CY, Lockwood CJ (2012). Queenan's Management of High-risk Pregnancy: An Evidence-based Approach. Vaginal Birth after Cesarean Section, West Sussex: Wiley-Blackwell, Chichester.
- Gary CF (2005) Obstetric Hemorrhage: Rupture of the Uterus, Williams Obstetrics. (23rdedn), McGraw-Hill Professional, New York.
- American College of Obstetricians and Gynecologists (2010) ACOG Practice bulletin no. 115: Vaginal birth after previous cesarean delivery. Obstetrics and Gynecology 116: 450-463.
- Berghella V, Airoldi J, O’Neill AM, Einhorn K, Hoffman M (2009) Misoprostol for second trimester pregnancy termination in women with prior caesarean: a systematic review. BJOG: An International Journal of Obstetrics & Gynaecology 116: 1151-1157.
- Sun HD, Su WH, Chang WH, Wen L, Huang BS, et al. (2012) Rupture of a pregnant unscarred uterus in an early secondary trimester: a case report and brief review. Journal of Obstetrics and Gynaecology Research 38: 442-445.
- Nur TE (2014) First Trimester Spontaneous Uterine Rupture in a Young Woman with Uterine Anomaly. Case Reports in Obstetrics and Gynecology.
- Mizutamari, Etsuko, Honda T, Ohba T, Katabuchi H (2014) Spontaneous Rupture of an Unscarred Gravid Uterus in a Primigravid Woman at 32 Weeks of Gestation. Case Reports in Obstetrics and Gynecology.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences