Mode of Delivery in a Woman with Multiple Brain Aneurysms
Ryutaro Yamada, Rina Akaishi, Mamoru Morikawa, Takahiro Yamada*, Takashi Kojima, Hisanori Minakami*
Ryutaro Yamada, Rina Akaishi, Mamoru Morikawa, Takahiro Yamada*, Takashi Kojima, Hisanori Minakami*
Department of Obstetrics, Hokkaido University Graduate School of Medicine, Japan
- Corresponding Author:
- Takahiro Yamada
Department of Obstetrics, Hokkaido University Graduate School of Medicine
N15W7, Kita-ku, Sapporo 060-8638, Japan
E-mail: taka0197@med.hokudai.ac.jp - Hisanori Minakami
Department of Obstetrics, Hokkaido University Graduate School of Medicine
N15W7, Kita-ku, Sapporo 060-8638, Japan
E-mail: minasho@med.hokudai.ac.jp
Received Date: March 23, 2016; Accepted Date: April 07, 2016; Published Date: April 14, 2016
Citation: Yamada K, Akaishi R, Morikawa M, et al. Mode of Delivery in a Woman with Multiple Brain Aneurysms. Crit Care Obst & Gyne. 2016, 2:2. doi: 10.21767/2471-9803.100021
Copyright: © 2016 Yamada R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
A 40-year-old pregnant woman with a family history of aneurysmal subarachnoid haemorrhage (aSAH) underwent magnetic resonance angiography (MRA). The MRA revealed two aneurysms (both measuring 4.0 mm) originating from both sides of the internal carotid artery in this patient, confirming the high prevalence rate of aneurysm with reported incidence of 25% among women with a family history of aSAH. Literature review suggested that advanced maternal age and family history of aSAH are risk factors for aSAH. Annual risk of aSAH is 0.95% for general Japanese patients with multiple small (<5 mm) unruptured aneurysms. Our analyses of published data suggested that the risk of aSAH was higher in the perinatal period compared to pregnancy remote from term. The patient elected to undergo prophylactic caesarean section.
Keywords
Brain aneurysm; Familial brain aneurysm; Mode of delivery; Prophylactic Caesarean section; Subarachnoid haemorrhage
Introduction
In two studies regarding the effects of pregnancy on the risk of intracranial aneurysm rupture [1,2], there is no evidence of an association between pregnancy and risk of aneurysm rupture, suggesting no need for elective caesarean section in women with asymptomatic un-ruptured intracranial aneurysms.
We encountered a pregnant woman with family history of brain haemorrhagic stroke and subarachnoid haemorrhage and were asked about a risk of brain haemorrhagic stroke associated with vaginal delivery. This case is presented with the consent of the patient and approval of the institutional review board of Hokkaido University Hospital. All work was conducted in accordance with the Declaration of Helsinki.
Case Report
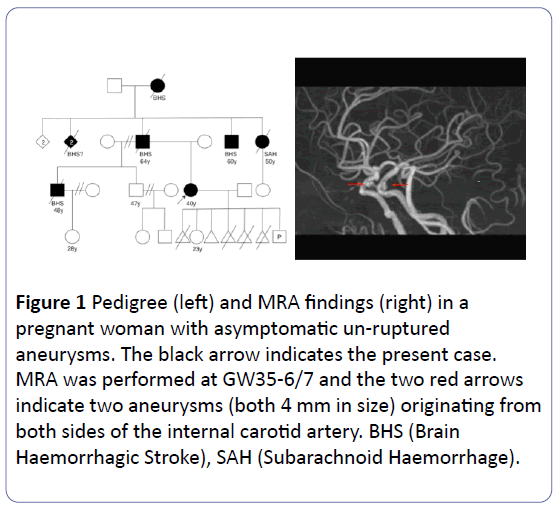
A 40-year-old Japanese woman with history of one previous childbirth at 17 years old and 5 abortions (1 spontaneous and 4 induced abortion) presented at gestational week (GW) 34-1/7. Her current pregnancy was uneventful, but her family history (Figure 1) and smoking habit prompted us to recommend magnetic resonance angiography (MRA) in this case, because 24% of females with a family history of subarachnoid haemorrhage (SAH) are detected to have intracranial aneurysm [3]. MRA performed at GW 35-6/7 revealed two aneurysms (both 4.0 mm in size) originating from both sides of the internal carotid artery (Figure 1). She did not develop hypertensive disorders of pregnancy, and gave birth to a healthy boy weighing 2,580 g by elective caesarean section at GW38-3/7 after extensive discussion about the risk of aSAH during vaginal delivery. The postpartum course was uneventful. With respect to size and shape, her aneurysms on postpartum days 8 and 171 were similar to those at GW 35-6/7.
Figure 1: Pedigree (left) and MRA findings (right) in a pregnant woman with asymptomatic un-ruptured aneurysms. The black arrow indicates the present case. MRA was performed at GW35-6/7 and the two red arrows indicate two aneurysms (both 4 mm in size) originating from both sides of the internal carotid artery. BHS (Brain Haemorrhagic Stroke), SAH (Subarachnoid Haemorrhage).
Discussion
As the outcome is poor once an intracranial aneurysm ruptures, the greatest concern is whether vaginal delivery will increase the risk of aneurysm rupture in women with known aneurysms.
The risk of aSAH is not increased in pregnancy compared to age-matched females—a study performed in Utrecht, indicated aSAH occurrence rates of 5.8 per 100,000 personyears (244 in 4,216,683 person-years) for non-pregnant women aged 18 – 42 years and 3.3 (7 in 214,490 person-years) for pregnant women [1]. However, this study did not take into consideration pregnancy stage for estimation of rupture risks [1]. Four (57%) of the seven cases of aSAH occurred on and after GW 38, and three occurred in the postnatal period within 11 days after birth in this previous study [1]. This phenomenon is seen worldwide: 87% of all of 707 hemorrhagic strokes occurred during parturition or postpartum in pregnant women in the USA [4]; 65% of all of 74 deaths from SAH occurred during parturition or postpartum in pregnant women in the UK [5]; two of three SAHs occurred postpartum in pregnant Taiwanese women [6]; and 57% of all of 13 aSAH occurred on GW 32 or later in pregnant Japanese women [7]. Thus, aneurysms may be most likely to rupture in a limited stage of pregnancy, i.e., during parturition and puerperium. Indeed in a Swedish cohort, the relative risk of SAH around delivery (from 2 days before to 1 day after delivery) was 46.9 (95% CI = 19.3 – 98.4) compared with unexposed (non-pregnant and early pregnant) women, and the risk of aneurysm rupture increased with advancing gestation [8]. The estimated incidence of SAH is approximately 15-fold higher for parturient and postpartum women than for pregnant women in the USA [9].
As both the circulating blood volume and the risk of aneurysm rupture increase with advancing gestation [8,10], the increased blood volume may be associated with the increased risk of aSAH. During parturition, 500 to 700 mL of blood is believed to move from the uterus to the general circulation with each labour pain. Retention of water in the interstitial space occurs physiologically in pregnancy. The process involved in the retention of water is reversed by parturition and excess water in the interstitial space returns into the intravascular space, causing expansion of the circulating blood postpartum, as evidenced by the decrease in haematocrit value postpartum [11]. Theoretically, therefore, circulatory instability is likely to occur during the perinatal period, especially in women undergoing vaginal delivery.
However, it is unclear at present whether elective caesarean section before onset of labour contributes to the avoidance of aSAH. The average annual risk of aSAH is 0.95% for Japanese patients with multiple small (<5 mm in size) unruptured aneurysms and several-fold higher than that of 0.95% for Japanese subjects with aneurysms ≥ 4.0 mm in diameter [12]. In addition, smoking, family history of SAH, and advanced maternal age are all risk factors of SAH/aneurysm rupture [3,8,13]. Therefore, our patient elected to undergo prophylactic caesarean section.
There is currently no evidence to support prophylactic caesarean section for the avoidance of aSAH. However, literature reports suggested that the risk of aSAH was higher in the perinatal period compared to pregnancy remote from term.
Disclosure
None have conflict of interest to declare.
References
- Groenestege ATT, Rinkel GJE, Bom JG, Algra A, Klijn CJM (2009) The risk of aneurysmal subarachnoid hemorrhage during pregnancy, delivery, and the puerperium in the Utrecht population. Stroke 40: 1148-1151.
- Kim YW, Neal D, Hoh BL (2013) Cerebral aneurysms in pregnancy and delivery: pregnancy and delivery do not increase the risk of aneurysm rupture. Neurosurgery 72: 143-150.
- Brown RD, Huston J, Hornung R (2008) Screening for brain aneurysm in the familial intracranial aneurysm study: frequency and predictors of lesion detection. J Neurosurg 108: 1132-1138.
- James AH, Bushnell CD, Jamison MG, Evan R, Myers ER (2005) Incidence and risk factors for stroke in pregnancy and the puerperium. ObstetGynecol 106:509-516.
- Foo L, Bewley S, Rudd A (2013) Maternal death from stroke: a thirty year national retrospective review. Eur J ObstetGynecolReprodBiol 171: 266-270.
- Jeng JS, Tang SC, Yip PK (2004) Incidence and etiologies of stroke during pregnancy and puerperium as evidenced in Taiwanese women. Cerebrovasc Dis 18: 290-295.
- Takahashi JC, Iihara K, Ishii A, Watanabe E, Ikeda T, Miyamoto S (2014) Pregnancy-associated intracranial hemorrhage: results of a survey of neurosurgical institutes across Japan. J Stroke Cerebrovas Dis 23:e65-e71.
- SalonenRos H, Lichtenstein P, Bellocco R, Petersson G, Cnattingius S (2001) Increased risks of circulatory diseases in late pregnancy and puerperium. Epidemiology 12:456-460.
- Bateman BT, Olbrecht VA, Berman MF, Minehart RD, Schwamm LH (2012) Peripartum subarachnoid hemorrhage: Nationwide data and institutional experience. Anesthesiology 116:324-333.
- Pritchard JA (1965) Changes in blood volume during pregnancy. Anesthesiology 26:393-399.
- Morikawa M, Yamada T, Akaishi R (2014) Gestational weight gain according to number of fetuses in Japanese women. J Perinat Med 42:523-538.
- Sonobe M, Yamazaki T, Yonekura M, Kikuchi, M (2010) Small unruptured intracranial aneurysm verification study SUAVe Study, Japan. Stroke 41:1969-1977.
- Okamoto K, Horisawa R (2007) Prediction of subarachnoid hemorrhage from a ruptured cerebral aneurysm by discriminant analysis in women. J Stroke Cerebrova Dis 16:245-250.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences