Recent Trends in Severe Maternal Morbidity (SMM) UPMC Harrisburg PA, 2016-2020
Catherine Baye Easton, Kendyl Schreiber, Yijin Wert, Holly Thomas, Brian Cohen, Abigail Lukasik and Courtney Potteiger
Catherine Baye Easton1*, Kendyl Schreiber2, Yijin Wert1, Holly Thomas1, Brian Cohen1, Abigail Lukasik1 and Courtney Potteiger1
1Department of Obstetrics and Gynecology, UPMC Harrisburg PA, United States
2Drexel University College of Medicine, Philadelphia PA, United States
- Corresponding Author:
- Catherine Baye Easton,
Department of Obstetrics and Gynecology UPMC
Harrisburg, PA, United Statess
E-mail: bayekate2@yahoo.com
Received date: April 24, 2021; Accepted date: April 14, 2021; Published date: April 30, 2021
Citation: Easton CB. (2021) Recent Trends in Severe Maternal Morbidity (SMM) UPMC Harrisburg PA, 2016-2020. Crit Care Obst Gyne Vol.7 No.3:32.
Abstract
Objectives: This study describes the current burden, trends and identifies the leading causes of Severe Maternal Morbidity (SMM) at UPMC Harrisburg Hospital. Additionally, the study provides recommendations for high priority, system-wide areas of improvement to advance the provision of maternal care.
Methods: This retrospective, population-based study analyzed SMM indicators as delineated by CDC guidelines and identified corresponding obstetric diagnosis and procedure codes from electronic medical records. The study population includes women with pregnancy and/or delivery-related hospitalizations within 42 days after delivery. The data was categorized by SMM indicator, maternal age, race/ethnicity, delivery mode, BMI, and transfusion.
Results: From October 2016 to October 2020, 479 patients experienced at least one SMM indicator. Blood transfusions were the most common (80%), followed by sepsis (3%), and HELLP and/or eclampsia (3%). There was a statistically significant difference in average maternal age between SMM patients with and without transfusions (28.7 vs. 30.8, p=0.0073). The study suggests that a higher BMI (≥30) is associated to 50% of the non-transfusion related morbidities. However, delivery mode is not a contributing factor.
Conclusion: Additional efforts are needed in this sector of public health given the increasing trends in maternal morbidity. Providing point-of-contact identification is critical to preventing maternal morbidity by SMM and requires adaptations to the present medical care system. Establishing a dedicated EMR database as the preferred medical record system for reporting and tracking SMM cases can streamline the process and help identify trending issues. Modifications to the database to allow simpler reporting of SMM indicators and patient trend analysis would benefit maternal care. There are multiple opportunities at the hospital level for reform and advancement to reduce the increasing rate of SMM.
Keywords
Severe maternal morbidity; Maternal health; Blood transfusions; ICD-10 codes
Abbreviations
ACOG: American College of Obstetricians and Gynecologists, ARDS: Acute Respiratory Distress Syndrome, BMI: Body Mass Index, CDC: Centers for Disease Control and Prevention, D and C: Dilation and Curettage, EMR: Electronic Medical Records, HELLP: Hemolysis Elevated liver Enzymes and Low Platelet Count Syndrome, HTN: Hypertension, ICD: International Classification of Diseases, OASIS: Obstetric Anal Sphincter Injuries, PPH-Postpartum Hemorrhage, pRBCs: Packed Red Blood Cells, QBL: Quantitative Blood Loss, SIRS: Systemic Inflammatory Response Syndrome, SMFM: Society for Maternal-Fetal Medicine, SMM: Severe Maternal Morbidity, TXA: Tranexamic Acid, UPMC: University of Pittsburgh Medical Center, VBAC: Vaginal Birth after Cesarean Delivery
Introduction
Severe Maternal Morbidity (SMM) remains a continuing threat against maternal health in the United States. While defined as any condition or diagnosis that could indicate a potentially life-threatening maternal complication, SMM encompasses various conditions including but not limited to cardiomyopathy, hemorrhage, organ failure, pregnancy-induced hypertension, seizure, pulmonary embolism, amniotic fluid embolism, sepsis and uterine rupture. This also includes unexpected outcomes of labor and delivery that result in significant short and/or longterm consequences to a woman’s health [1]. In the absence of prompt identification and treatment, these conditions can lead to maternal death [2,3].
A recent CDC report showed that SMM has been steadily increasing in recent years and affected more than 50,000 women in the United States in 2014 [4-6]. According to the CDC Pregnancy Mortality Surveillance System, pregnancy-related deaths per 100,000 births have steadily increased from 7.2 deaths in 1987 to 17.3 deaths in 2017 [7]. These numbers may be understated as there is still not a complete consensus on the defined conditions which are associated with SMM [1]. Additionally, there is not a standardized set of diagnostic codes to facilitate accurate SMM surveillance. It is difficult to precisely define the reasons for this drastic increase in pregnancy-related deaths. There are indications that should be considered; this includes more consistent identification and recording of these deaths as technology and hospital coding practices have improved [8].
With declining maternal mortality in high income countries, the concept of SMM has become more relevant in small geographic regions and is utilized as an indicator of the quality of maternal health [5,6,9]. The impact of SMM cannot be stressed enough as maternal morbidity is traumatic and affects the woman’s physical and mental health, her family, and friends, as well as the overall community. For example, women who experience SMM may be at increased risk of post-traumatic stress disorder symptoms during the 6-8 weeks (about 2 months) after delivery [10].
Moreover, subsequent hospitalizations during the year after delivery are higher for women who experience SMM, even when those with preexisting chronic conditions are excluded [11]. Women with SMM may have an increased likelihood for emergency department visits up to 90 days after delivery [12]. For example, women with hypertensive disorders of pregnancy had higher hospitalization readmission rates for cardiovascular disease [13]. Healthcare systems are impacted by SMM as well. One study found that hospital cost in 2011-2012 for patients with SMM was 2.1 times higher than in patients without SMM [14]. Subsequent studies reported a doubling of costs associated with delivery in patients with SMM [15-17].
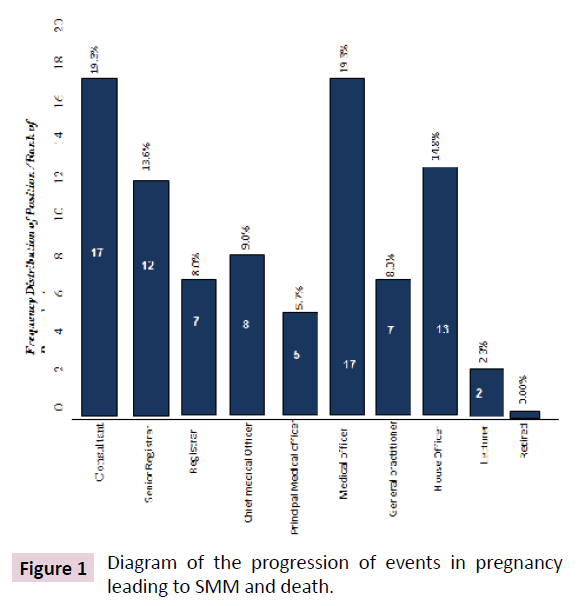
The concept of using SMM as a basis for quality and system-wide recommendations follows the sequence of events from a normal healthy pregnant population to pregnancy-related mortality as shown in Figure 1 [18]. Improving the health of the pregnant population by identifying and acting upon the middle tier issues prevents the bottom tier which is death in the pregnant population.
Methods
Population
This study was conducted to analyze the trends and patterns in severe maternal morbidity in patients at UPMC Harrisburg Hospital during the four-year period of October 1, 2016, to October 1, 2020. The UPMC Harrisburg Hospital has an average of 4,900 deliveries each year of which approximately 30% are Cesarean deliveries, 70% are vaginal deliveries 9 including operative vaginal deliveries and VBAC. The subjects considered in the study were women with pregnancy and/or delivery-related hospitalizations including 42 days after delivery and identified as having experienced an SMM event using the CDC updated list of 21 indicators and the International Classification of Diseases (ICD- 9 and ICD-10) diagnosis and procedure codes from administrative hospital discharge data Table 1. were used [19,20]. Due to the rare prevalence, some indicators (for example, issues pertaining to the vascular system) were grouped together. The unit of analysis was the identified SMM indicator, not the individual.
Table 1: Indicators of severe maternal morbidity.
| CDC Indicators of Severe Maternal Morbidity | |
| Acute myocardial infarction | Pulmonary edema/acute heart failure |
| Aneurysm | Severe anesthesia complications |
| Acute renal failure | Sepsis |
| Adult Respiratory distress syndrome | Shock |
| Amniotic fluid embolism | Sickle cell disease (trait) with crisis |
| Cardiac arrest/ventricular fibrillation | Air and thrombotic embolism |
| Dysrhythmia or Arrythmia | Blood products transfusion |
| Disseminated intravascular coagulation | Hysterectomy |
| Eclampsia | Temporary tracheostomy |
| Heart Failure/arrest during surgery or procedure | Ventilation |
| Puerperal cerebrovascular disorders | - |
Data Sources
The study population’s information was obtained from Electronic Medical Records (EMRs) acquired from the hospital’s EPIC database (Epic Systems Corporation, Verona, WI). All data and records generated through the study were kept confidential and in alignment with UPMC institutional research policies. Furthermore, the study was reviewed and approved by the UPMC Institutional Review Board (IRB). It was conducted in accordance with UPMC human subjects’ research requirements as well as applicable federal regulations. As this was a retrospective analysis of health records. No contact occurred with the women whose information was included in the study.
Analysis
The severe maternal morbidity rate was calculated as the number of women identified with an SMM indicator per 1,000 delivery hospitalizations. The leading SMM indicators were reported as a rate per 10,000 delivery hospitalizations. Demographic metrics for the descriptive analysis included age, race/ethnicity, Body Mass Index (BMI), and delivery mode (C-section or vaginal delivery). These data and distributions were then compared with the occurrence of SMM with and without blood transfusions. Chi-square tests were used to detect statistical significance for the categorical variables and a student t-test was used for the continuous variable. A p-value of less than 0.05 was considered for statistical significance. All the analyses were performed using in SAS® software, version 9.4 (SAS Institute, Cary, NC).
Results
From October 1, 2016, to September 30, 2020, a total of 479 SMM cases were reported at UPMC Harrisburg Hospital. The distribution of identified SMM indicators is tabulated in Table 2. Blood transfusions were the most common indicator of SMM and contributed to 80% (n=382) of all SMM cases, followed by sepsis 3% (n=12)and hemolysis, elevated liver enzymes, and low platelet count syndrome (HELLP) and/or eclampsia 3% (n=15).
Table 2: Severe maternal morbidity case distribution 2016-2020.
| SMM Category | Number of Cases | Percent of Cases |
|---|---|---|
| Blood transfusion | 382 | 79.75% |
| Sepsis | 12 | 3.34% |
| HELLP and/or eclampsia | 15 | 3.13% |
| Cardiac complications | 14 | 2.92% |
| Pulmonary embolism | 8 | 1.67% |
| Hysterectomy | 8 | 1.67% |
| Puerperal cerebrovascular disorders | 7 | 1.46% |
| Aneurysm | 7 | 1.46% |
| Acute pulmonary edema/ARDS | 7 | 1.46% |
| Acute renal failure | 6 | 1.25% |
| Shock | 4 | 0.84% |
| Amniotic fluid embolism | 2 | 0.42% |
| Anesthesia complication | 2 | 0.42% |
| Sickle cell disease with crisis | 1 | 0.21% |
HELLP: Hemolysis Elevated Liver Enzymes, and Low Platelet Count Syndrome, ARDS: Acute Respiratory Distress Syndrome.
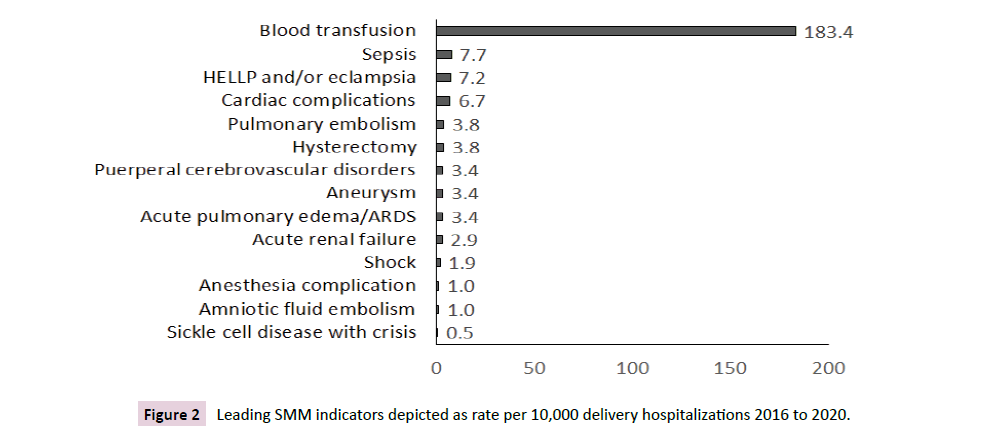
When assessed per 10,000 delivery hospitalizations, rate for blood transfusions dramatically outnumbered other indicators at 183.4 patients followed by rates for sepsis and HELLP and/or eclampsia at 7.7 and 7.2 patients, respectively Figure 2.
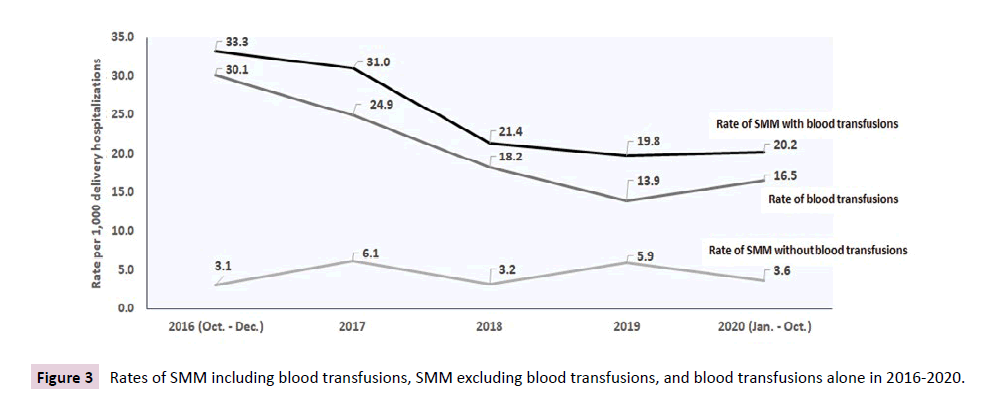
The overall rate of SMM decreased by 39.4% over the study period, with rates decreasing from 33.3 in 2016 to 20.2 in 2020. This decrease has been driven primarily by the overall rate of blood transfusions decrease from 30.1 to 16.5. Excluding blood transfusions as a factor, the rate of SMM increased over time, from 3.1 to 3.6 Figure 3.
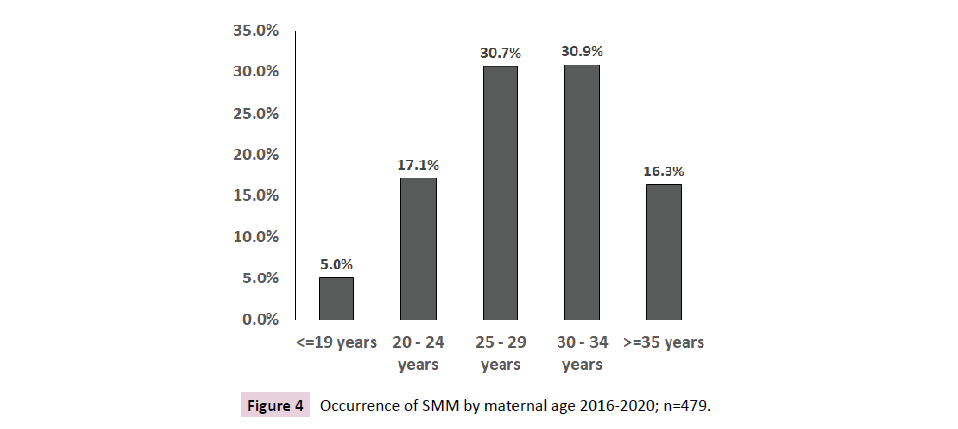
The occurrence of SMM was categorized by maternal age. Most patients (60%) were between 25 and 34 years old Figure 4. There was a statistically significant difference in average age between SMM patients with blood transfusions and SMM patients without transfusions (28.7 vs. 30.8, p=0.0073) Table 3.
Table 3: Occurrence of SMM (including blood transfusions), SMM (excluding blood transfusions), and overall blood transfusions among maternal age categories.
| SMM (including blood transfusions) | SMM (excluding blood transfusions) | Blood Transfusions | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| Total number of patients | 479 | 97 | 382 | 0.0011 | ||||
| Age-Mean (SD), Range | 29.1 (5.8) | 13-45 | 30.8 (5.7) | 17-44 | 28.7(5.8) | 13-45 | 0.0073 | |
| Age Category | ||||||||
| ≤19 years | 24 | 5.00% | 5 | 5.20% | 19 | 5.00% | ||
| 20-24 years | 82 | 17.10% | 8 | 8.20% | 74 | 19.40% | ||
| 25-29 years | 147 | 30.70% | 23 | 23.70% | 124 | 32.50% | ||
| 30-34 years | 148 | 30.90% | 39 | 40.20% | 109 | 28.50% | ||
| ≥35 years | 78 | 16.30% | 22 | 22.70% | 56 | 14.70% | ||
Taking blood transfusions into account as an SMM indicator, there was a statistically significant difference between SMM patients with blood transfusions and SMM patients without transfusions Table 3.
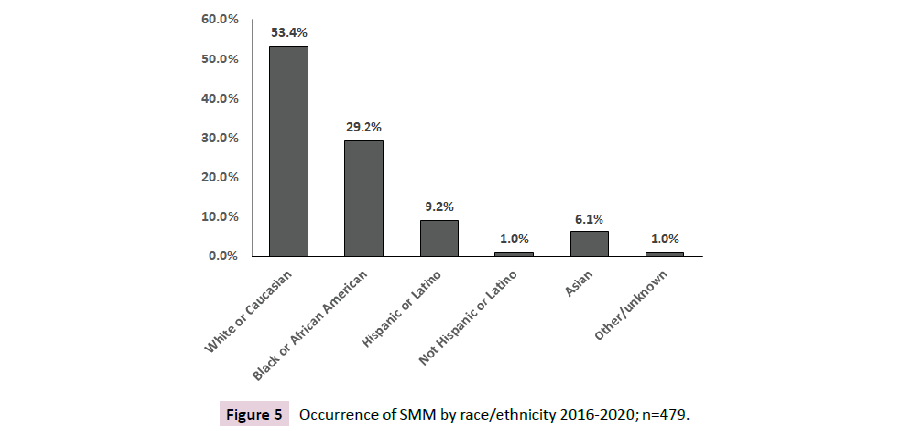
The impact of maternal race and ethnicity on severe maternal morbidity was examined. Of note was 53.4% of SMM patients identified as white or Caucasian Figure 5.
In 57% of SMM cases, patients delivered via cesarean section. There was no statistically significant difference (p-value= 0.1345) in delivery modes between SMM with and without blood transfusions (Table 4). Table 5 further details the SMM indicators based on delivery mode.
Table 4: Occurrence of SMM by delivery mode 2016-2020.
| SMM (including blood transfusions) | SMM (excluding blood transfusions) | Blood transfusions | p-value | ||||
|---|---|---|---|---|---|---|---|
| Total number of patients | 479 | 97 | 382 | 0.1345 | |||
| C-section | 274 | 57.20% | 62 | 63.90% | 212 | 55.50% | - |
| Vaginal delivery | 205 | 42.80% | 35 | 36.10% | 170 | 44.50% | - |
Table 5: Occurrence of identified SMM indicators by delivery mode.
| SMM Category | C-section | Vaginal Delivery | ||
|---|---|---|---|---|
| Total number of patients | 274 | 205 | ||
| Acute pulmonary edema/ARDS | 6 | 2.20% | 1 | 0.50% |
| Acute renal failure | 6 | 2.20% | 0 | 0.00% |
| Amniotic fluid embolism | 2 | 0.70% | 0 | 0.00% |
| Anesthesia complication | 1 | 0.40% | 1 | 0.50% |
| Aneurysm | 2 | 0.70% | 5 | 2.40% |
| Cardiac complications | 7 | 2.60% | 7 | 3.40% |
| HELLP and/or eclampsia | 12 | 4.40% | 3 | 1.50% |
| Hysterectomy | 7 | 2.60% | 1 | 0.50% |
| Puerperal cerebrovascular disorders | 3 | 1.10% | 4 | 2.00% |
| Pulmonary embolism | 4 | 1.50% | 4 | 2.00% |
| Sepsis | 7 | 2.60% | 9 | 4.40% |
| Shock | 4 | 1.50% | 0 | 0.00% |
| Sickle cell disease with crisis | 1 | 0.40% | 0 | 0.00% |
| Blood transfusion | 212 | 77.40% | 270 | 82.90% |
Examining the SMM case distribution by BMI category, the study suggested that a higher BMI (≥25) does contribute to 50% of the non-transfusion related morbidities Table 6.
Table 6: Occurrence of SMM categorized by BMI.
| Total number of patients | SMM (including blood transfusions) | SMM (excluding blood transfusions) | Blood Transfusions | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| 479 | 97 | 382 | 0.375 | |||||
| BMI Category | <18.5 Underweight | 16 | 3.30% | 5 | 5.20% | 11 | 2.90% | - |
| 18.5-24.9 Normal | 111 | 23.20% | 17 | 17.50% | 94 | 24.60% | - | |
| 25.0-29.9 Overweight | 132 | 27.60% | 26 | 26.80% | 106 | 27.70% | - | |
| 30.0-34.5 Obesity (Class I) | 102 | 21.30% | 20 | 20.60% | 82 | 21.50% | - | |
| 35.0-39.9 Obesity (ClassII) | 70 | 14.60% | 15 | 15.50% | 55 | 14.40% | - | |
| >40 Obesity (Class III) | 48 | 10.00% | 14 | 14.40% | 34 | 8.90% | - | |
Discussion
Taken together, the present study shows similar trends to those observed in other studies in the United States. However, these observations are likely only a limited proportion of the total burden of pregnancy, labor, and delivery complications faced by women. From October 1, 2016, to October 1, 2020, a total of 479 patients in this study suffered at least one of the indicators of SMM with the top three indicators of SMM being blood transfusion, sepsis, and HELLP and/or eclampsia. Specific measures can be recommended to reduce the number of women experiencing these concerns. Identified as the top SMM indicator, this study dissociated the rate of blood transfusions from the overall rate of SMM to show that while the overall rate of SMM decreased by almost 40% during the study period. This trend was primarily driven by the overall decrease of blood transfusions given; moreover, when the data for blood transfusions is separated out, it shows that total observations of SMM continue to increase. Thus, it remains important to understand the individual aspects of SMM so as not to obscure underlying trends.
This distribution supports the results found in a similar study by Assibey Menshah et al. wherein blood transfusions constituted 66% of all SMM cases as the most common indicator with a rate of 13.8 per 1,000 deliveries in Philadelphia Country [21]. CDC data notes that the top three indicators of SMM are blood transfusions, cesarean hysterectomy, and temporary tracheostomy [22]. The CDC reported an overall SMM rate (including blood transfusions) of 14.4, an overall blood transfusion rate of 12.2, and an SMM rate (excluding blood transfusions) of 3.5 in 2014 using data acquired from the National (Nationwide) Inpatient Sample databases [23]. In a study of SMM in Massachusetts, Harvey et al used the Pregnancy to Early Life Longitudinal data system which links birth/fetal death records with hospital discharge records, at noted an average SMM rate of 9.9 per 1,000 deliveries between 2002 to 2011 [24]. Additionally, Assibey Menshah et al. noted a SMM rate of 22.7 per 1,000 deliveries in 2014 in Philadelphia Country [21].
Of the study population, most patients who experienced SMM were between 25 and 34 years old (61.6%). When assessing whether this majority was more susceptible to SMM, the data demonstrated that there was a statistically significant difference in women of this age range that cannot be attributed to blood transfusions alone.
On initial analysis, white or Caucasian women comprised 53.4% of the affected population, followed by black or African American women at 29.2%. However, given that 67% of our patient population are White or Caucasian and 21% are black or African American, our study does seem to align with other studies which have shown higher rates of SMM among non-Hispanic black women when compared to Caucasian women [25,26]. Given the limited scope of this study, no definitive conclusions can be drawn from this data. Other studies have shown SMM to be more frequent among women who give birth by cesarean section, as cesarean delivery carries more risk of maternal complications [27]. In this study, after dissociating the data for blood transfusions alone, there was no conclusive evidence within this population to show that there was a difference between vaginal and cesarean delivery in terms of SMM. However, obesity is a contributing factor to non-blood transfusion related morbidities. In cases of pregnancy in women with a BMI ≥ 30.0, additional attention, and monitoring should be placed on their health vitals to detect SMM indicators early to mitigate preventable adverse outcomes. Including additional prenatal discussions addressing the risk factors of a higher BMI may further increase patient awareness of gestational weight gain.
The trends observed in blood transfusions could benefit from implementing revised patient blood management practices throughout pregnancy. Patient blood management which aims to improve patient outcome and safety by reducing the number of unnecessary Red Blood Cell (RBC) transfusions and vitalizing patient-specific anemia reserves. Certain areas that could benefit from additional medical supervision include optimizing pre-pregnancy hematocrit and hemoglobin levels and ensuring adequate blood iron levels during pregnancy. Other studies have documented how pregnancy substantially decreases hemoglobin concentration, and routine blood screenings during pregnancy could be very beneficial to identifying issues prior to crisis [28]. As iron is an essential microelement in maternal health, iron supplementation and intravenous iron infusions during pregnancy may also provide a benefit to women at risk for SMM [29].
Data suggests that obstetric hemorrhage, a leading cause for blood transfusion, accounts for most maternal deaths, but 54% to 93% of these deaths are preventable [30-33]. Thus, improvement in maternal care and departmental practices may reduce these unnecessary deaths. Based on the high rates of transfusions observed, we recommend providing continuing education on the prevention of Postpartum Hemorrhage (PPH), Quantitative Blood Loss (QBL), the use of uterotonics, and timing of PPH identification. Furthermore, early administration of Tranexamic Acid (TXA) and fibrinogen concentrate to manage PPH should be considered as well as focusing on rapid diagnosis and correction of coagulopathy in pregnant patients. In addition to the previous recommendations, intra-operative cell salvage may be considered for its obstetric potential to treat patients safely and effectively with predicted potential for massive obstetric hemorrhage [33,34].
Among the most common indicators, sepsis can be more effectively managed through prompt identification and infection treatment in the peripartum period as research has shown that over 30% of sepsis cases were impacted by delayed recognition [35]. Specifically, preventative measures include more research and institutional standardization of prophylactic antibiotic use following operative deliveries, Obstetric Anal Sphincter Injuries (OASIS), manual removal of the placenta, postpartum Dilation and Curettage (D and C), and PPH [36]. Eclampsia, including HELLP syndrome, also continues to be a leading indicator of SMM, one of which results in many preventable cases. In terms of recommendations to reduce these events, Hypertension (HTN) management is a critical matter requiring immediate management [37]. In particular, prompt evidence-based management of gestational hypertension along with continuing clinical education on severe HTN management protocols can decrease the number of fatal cases. Following delivery, women who have risk factors for pre-eclampsia should be offered short and long-term HTN management options including closer postpartum visits, home blood pressure monitoring and multi-disciplinary team management as needed. Notably, some limitations of this study can be areas for improvement in the medical care system. In general, navigating through and collecting data on the relevant patients in the EPIC electronic medical record database was labor intensive and not conducive to supporting data and trend analysis in patient care. In part, this stemmed from issues extracting the ICD codes from administrative data which is not designed with research in mind; additionally, much of the available patient data could have been improved with more thorough documentation as well as added validity and oversight to the data content. This study demonstrates the increased need to investigate trends relating to maternal health to prevent SMM. In particular, the leading indicators of SMM continue to be blood transfusions, sepsis, and HELLP/eclampsia.
The results of this study further demonstrate the inadequacies present in maternal care which, if addressed, will reduce the many cases of preventable maternal morbidity. The recommendations discussed herein describe a revised agenda focusing on prompt, evidence-based identification, and management of SMM indicators which begins with updated clinical practices and continuing education. Furthermore, establishing EMR databases modified to document SMM indicators/risk factors and increase the ease of data reporting may also provide in-time information for addressing these issues at the hospital level. In addition, improved analysis of patient data will also help identify SMM hospitalizations that occur outside of delivery hospitalizations, including antepartum and postpartum issues as this period may account for additional SMM cases not previously considered.
SMM. We need to accurately define SMM and then standardized criteria to identify women at risk of having a severe maternal morbidity event. Utilizing these criteria, we can then build them into our EMR systems to work for us by flagging our OB providers and by having the ability to capture data for further study. Changing our postpartum follow-up for SMM patients can also benefit and lastly, improving access and coverage to our moms to decrease SMM. Specifically, establishing a dedicated EMR database for reporting and tracking SMM cases can streamline the process and help identify trending issues. Modifications to the database to allow simpler reporting of SMM indicators and patient trend analysis would be beneficial to improving care. Identifying an outcome as a severe maternal morbidity does not suggest blame, nor does it mean that there will always be an opportunity for improvement. Reviewing such cases in detail to determine whether the morbidity may have been avoidable and whether it should prompt changes in systems for care provision is, however, a necessary and crucial step in efforts to ensure quality obstetric care. Patient education and encouragement will continue to be a necessary point of focus for improving SMM trends. This begins with informing women on the necessity to always identify as pregnant or previously pregnant when seeking medical care within the last year. Increasing awareness at the community level of the importance of preconception, prenatal, and postpartum care can make a difference in initiating the necessary conversations in the medical setting.
Insurance and payer policies may also be important to include in future research in terms of trends and rates of SMM; women who are not fully covered by insurance may not seek the critical care needed to prevent SMM events. Thus, campaigning for policy changes to promote greater access to essential maternal care is key to ensuring that at-risk pregnant and postpartum women are connected to and able to afford subspecialty care. Thus, tracking and understanding current patterns of SMM, along with developing and carrying out interventions to improve the quality of maternal care are essential to reducing SMM.
In summary we recommend several process changes to decrease SMM. We need to accurately define SMM and then standardized criteria to identify women at risk of having a severe maternal morbidity event. Utilizing these criteria, we can then build them into our EMR systems to work for us by flagging our OB providers and by having the ability to capture data for further study. Changing our postpartum follow-up for SMM patients can also benefit and lastly, improving access and coverage to our moms to decrease SMM.
Acknowledgments
We would like to thank the faculty and staff at the UPMC Harrisburg OB-GYN residency program who are helping our new class of OB-GYN residents’ support and enhance the lives of girls and women in our community. We also appreciate the library staff at UPMC Harrisburg Hospital, especially Laurie Schwing who provided guidance all through and final review of this manuscript.
Funding/Conflicts of Interests
The authors have declared that no competing or financial interests exist. This research study did not receive any specific grant from funding agencies in the public, commercial, or not-forprofit sectors.
References
- Kilpatrick SK, Ecker JL (2016) Obstetricians ACo, gynecologists: severe maternal morbidity: screening and review. Am J Obstet Gynecol 3: B17-B22.
- Schockaert S, Poppe W, Arbyn M, Verguts T, Verguts J (2008) Incidence of vaginal intraepithelial neoplasia after hysterectomy for cervical intraepithelial neoplasia: a retrospective study. Am J Obstet Gynecol 2: 113-e1.
- Kyser KL, Lu X, Santillan DA, Santillan MK, Hunter SK, et al. (2012) The association between hospital obstetrical volume and maternal postpartum complications. Am J Obstet Gynecol 1: 42-e1.
- Kozhimannil KB, Interrante JD, Henning-Smith C, Admon LK (2019) Rural-urban differences in severe maternal morbidity and mortality in the US, 2007–15. Health affairs 12: 2077-2085.
- Callaghan WM, Creanga AA, Kuklina EV (2012) Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol 5: 1029-1036.
- Danel I, Berg C, Johnson CH, Atrash H (2003) Magnitude of maternal morbidity during labor and delivery: United States, 1993-1997. Am J Public Health 4: 631-634.
- Douthard RA, Martin IK, Chapple-McGruder T, Langer A, Chang S (2021) US maternal mortality within a global context: Historical trends, current state, and future directions. J Women's Health 2: 168-177.
- Baeva S, Saxton DL, Ruggiero K, Kormondy ML, Hollier LM, et al. (2018) Identifying maternal deaths in Texas using an enhanced method, 2012. Obstet Gynecol 5: 762-769.
- World Health Organization (2019) Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division.
- Furuta M, Sandall J, Cooper D, Bick D (2014) The relationship between severe maternal morbidity and psychological health symptoms at 6-8 weeks postpartum: a prospective cohort study in one English maternity unit. BMC Pregnancy and Childbirth 1: 1-14.
- Harvey EM, Ahmed S, Manning SE, Diop H, Argani C, et al. (2018) Severe maternal morbidity at delivery and risk of hospital encounters within 6 weeks and 1 year postpartum. J Women's Health 2: 140-147.
- Batra P, Fridman M, Leng M, Gregory KD (2017) Emergency department care in the postpartum period: California births, 2009-2011. Obstet Gynecol 5: 1073-1081.
- Jarvie JL, Metz TD, Davis MB, Ehrig JC, Kao DP (2018) Short-term risk of cardiovascular readmission following a hypertensive disorder of pregnancy. Heart 14: 1187-1194.
- Chen HY, Chauhan SP, Blackwell SC (2018) Severe maternal morbidity and hospital cost among hospitalized deliveries in the United States. Am J Perinatol 13: 1287-1296.
- Nam JY, Cho E, Park EC (2019) Do severe maternal morbidity and adequate prenatal care affect the delivery cost? A nationwide cohort study for 11 years with follow up. Int J Gynaecol Obstet 13: 1623-1631.
- Austin AE, Gottfredson NC, Zolotor AJ, Halpern CT, Marshall SW, et al. (2020) Preconception and Prenatal Predictors of Early Experiences of Risk and Protection Among Alaska Children. Matern Child Health J 1: 82-89.
- Howland RE, Angley M, Won SH, Wilcox W, Searing H, et al. (2018) Estimating the hospital delivery costs associated with severe maternal morbidity in New York City, 2008–2012. Obstet Gynecol 2: 242-252.
- Mantel GD, Buchmann E, Rees H, Pattinson RC (1998) Severe acute maternal morbidity: a pilot study of a definition for a near‐miss. Int J Gynaecol Obstet 9: 985-990.
- Say L, Souza JP, Pattinson RC (2009) Maternal near miss–towards a standard tool for monitoring quality of maternal health care. Best Pract Res Clin Obstet Gynaecol 3: 287-296.
- Kozhimannil KB, Interrante JD, Henning-Smith C, Admon LK, (2019) Rural-urban differences in severe maternal morbidity and mortality in the US, 2007–15. Health affairs 12: 2077-2085.
- Assibey MV, Huynh MP, Todd M, (2014) Severe Maternal Morbidity in Philadelphia, Calculations Brief #1. February 2020. Philadelphia Department of Public Health, Philadelphia PA pp:1-7.
- Tangel VE, Matthews KC, Abramovitz SE, White RS, (2020) Racial and ethnic disparities in severe maternal morbidity and anesthetic techniques for obstetric deliveries: A multi-state analysis, 2007-2014. J Clin Anesth 65: 109821.
- Fingar KR, Hambrick MM, Heslin KC, Moore JE (2018) Trends and disparities in delivery hospitalizations involving severe maternal morbidity, 2006-2015: statistical brief# 243.
- Harvey EM, Ahmed S, Manning SE, Diop H, Argani C (2018) Severe maternal morbidity at delivery and risk of hospital encounters within 6 weeks and 1 year postpartum. J Women's Health 2: 140-147.
- Admon LK, Winkelman TN, Zivin K, Terplan M, Mhyre JM, et al. (2018) Racial and ethnic disparities in the incidence of severe maternal morbidity in the United States, 2012-2015. Obstet Gynecol 5: 1158-1166.
- Creanga AA, Bateman BT, Kuklina EV, Callaghan WM (2014) Racial and ethnic disparities in severe maternal morbidity: a multistate analysis, 2008-2010. Am J Obstet Gynecol 5: 435-e1.
- Pallasmaa N, Ekblad U, Gissler M, (2008) Severe maternal morbidity and the mode of delivery. Acta Obstet Gynecol Scand 6: 662-668.
- Feleke BE, Feleke TE (2020). The Effect of Pregnancy in the Hemoglobin Concentration of Pregnant Women: A Longitudinal Study. J pregnancy 2020: 1-6.
- Grzeszczak K, Kwiatkowski S, Kosik BD (2020) The role of Fe, Zn, and Cu in pregnancy. Biomolecules 8: 1176.
- Burtelow M, Riley E, Druzin M, Fontaine M, Viele M, et al. (2007) How we treat: management of life‐threatening primary postpartum hemorrhage with a standardized massive transfusion protocol. Transfusion 9: 1564-1572.
- Berg C, Harper M, Atkinson S (2005) The North Carolina maternal mortality review committee. Obstet Gynecol 6: 1228-1234.
- Della TM, Kilpatrick SJ, Hibbard JU, Simonson L, Scott S, et al. (2011) Assessing preventability for obstetric hemorrhage. Am J Perinatol 4: 531-539.
- Liu Y, Li X, Che X, Zhao G, Xu M (2020) Intraoperative cell salvage for obstetrics: a prospective randomized controlled clinical trial. BMC Pregnancy Childbirth 1: 1-8.
- Sullivan IJ, Ralph CJ (2019) Obstetric intra‐operative cell salvage: a review of an established cell salvage service with 1170 re‐infused cases. Anaesthesia 8: 976-983.
- Lepine S, Lawton B, Geller S, Abels P, MacDonald EJ (2018) Severe maternal morbidity due to sepsis: The burden and preventability of disease in New Zealand. Australian and New Zealand. J Obstet Gynecol 6: 648-653.
- Foeller ME, Gibbs RS (2019) Maternal sepsis: new concepts, new practices. Curr Opin Gynecol Obstet 2: 90-96.
- Sutton AL, Harper LM, Tita AT (2018) Hypertensive disorders in pregnancy. Obstet Gynecol Cli 2: 333-347.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences