Laparoscopic Excision Ablation or Ablation Alone in Women with Endometrioma
Nahed Ezzat Allam, Taiseer Maarouf Mohamed and Eman Ibrahiem Ahmed
DOI10.21767/2471-9803.1000161
Department of Obstetrics and Gynaecology, Faculty of Medicine, Al-Azhar University Hospital, Cairo, Egypt
- Corresponding Author:
- Nahed Ezzat Allam
Department of Obstetrics and Gynaecology
Faculty of Medicine, Al-Azhar University Hospital
Cairo, Egypt
Tel: 01121116136
E-mail: nahedallam16@gmail.com
Received Date: July 04, 2018; Accepted Date: July 25, 2018; Published Date: July 31, 2018
Citation: Allam NE, Mohamed TM, Ahmed EI (2018) Laparoscopic Excision Ablation or Ablation Alone in Women with Endometrioma. Crit Care Obst Gyne. Vol.4 No.2:8. doi:10.21767/2471-9803.1000161
Copyright: © 2018 Allam NE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Effect of laparoscopic intervention in management of endometriomas could be associated with a deleterious effect on ovarian function.
Objective: To compare the effect of laparoscopic ablation excision and ablation alone in patients with unilateral mild to moderately sized endometrioma on Antral Follicle Count (AFC), ovarian volume, day 2 FSH (D2 FSH).
Method: Clinical randomized trial carried out on 62 patients was randomly allocated to,
Group A: 31 patients where combined laparoscopic excision/ablation,
Group B: 31 patients where laparoscopic ablation was done.
Primary outcomes: AFC, D2 FSH and ovarian volume.
Results: The range of age in both groups was 22-36 years, demographic data and endometrioma size were comparable, patients in group A was presented mainly by pain and secondary infertility while in group B, the main complaint was primary infertility. FSH showed statistically significant difference after 3 months (Median=5.85 versus 5, P value 0.004) and statistically significant difference found between both groups regarding AFC 6 months postoperative where the AFC decreased more in patients managed by ablation alone. Also, statistical significant difference found between groups regarding volume of ipsilateral ovary 6 months post-operative where the volume decreased more in patients managed by ablation (Median=11 versus 6.25 cm3, P value 0.003), no statistical significant difference found between the two studied groups regarding pregnancy or recurrence rate 3 and 6 months post-operative.
Conclusion: Both laparoscopic excision ablation or ablation alone for management of unilateral endometrioma ≤ 5 cm decreased ovarian volume of ipsilateral ovary and improved serum FSH level but slightly increased AFC. Ablation alone had more negative impact on ovarian volume and AFC.
Keywords
Laparoscopy; Ovarian volume; Day 2 FSH
Abbreviations
AFC: Antral Follicle Count; IVF: In-Vitro Fertilisation; FSH: Follicle-Stimulating Hormone; AMH: Anti-Mullerian Hormone
Introduction
Laparoscopy is considered the gold-standard treatment for ovarian endometriomas [1]. Many reports mentioned different techniques that may be used as, cystic wall laser vaporization, drainage and bipolar coagulation of the cystic wall and endometrioma stripping; however, debates still happening and we do not know which one is the most effective at avoiding ovarian damage. Surgery can lead to a reduction in OR by three main mechanisms:
1) Excessive stripping of the ovarian cortex,
2) The use of bipolar coagulation to stop bleeding and,
3) The presence of surgery-induced inflammation [1,2].
There has been increasing evidence that ovarian responsiveness drops after any surgical treatment for ovarian endometrioma but, potential reduction in ovarian reserve attributed to surgery should be considered in women with bilateral disease, asymptomatic disease and those undergoing In-Vitro Fertilisation (IVF) [3]. Aim is to compare effect of two laparoscopic techniques on AFC, ovarian volume and D2 FSH serum level.
Participants and Methods
A clinical double-blind randomized trial was conducted in Obstetrics and Gynaecology Department, Al-Azhar University Hospital in the period between April 2016 and March 2018, for women with unilateral or bilateral ovarian endometrioma. After admission women were assigned after computer randomization to either one of the two treatment protocols.
Study participants: 62 women presented with primary, secondary infertility or chronic pelvic pain with pre-existing unilateral or bilateral ovarian endometrioma. Sample size was adjusted according to the equation:
N={(a+b)2 (p1q1+p2q2)}/ x2 [4]
Inclusion criteria: 19< Age <40 years, 18.5 kg/m2< BMI <35 kg/m2, size of the endometrioma from 4-8 cm non-infiltrating lesions.
Exclusion criteria: History of previous surgery for adnexal pathology, contraindication for laparoscopy. Each patient subjected to full history taking (personal history, menstrual, sexual and gynaecological history). Past history both medical and surgical.
Physical examination: (general, abdominal and pelvic examination). 2D trans-vaginal ultrasonography (GE VolusonS6) post-menstrual to confirm size and number of endometrioma in addition to ovarian reserve indices for ipsilateral and contralateral side (AFC and ovarian volume - D2 FSH). These patients assigned by doctor in duty other than authors and randomly allocated using shuffling cards to groups: Group A included 31 women for combined laparoscopic excision/ablation technique. Group B included 31 women for laparoscopic ablation electrocoagulation surgical current. Both patients and assessor (third author) were blinded to the treatment protocol. No medical treatment given, each women scheduled for 2 follow up visits in 3 and 6 months after the operation and post menstrual, where trans-vaginal (2D) ultrasonography done to estimate ovarian reserve function in both sides using AFC, ovarian volume and D2 FSH and to detect recurrence (recurrent endometriotic cyst and or pain) and any changes in the ovarian reserve markers as primary outcome and conversion from planned laparoscopic procedure to laparotomy, post-operative complications and pregnancy and recurrence rates (+ve pregnancy test and early fetal viability) as secondary outcomes.
Laparoscopic operations were performed with three 5-mm trocars in the lower abdomen and a 10 mm Intra umbilical main trocar. We used 5 mm scissors and graspers, and normal saline solution for irrigation.
In group A and after identification of the cleavage plane, the wall of the cyst was stripped off healthy ovarian tissue with two a-traumatic grasping forceps. After removing most of the pseudo capsule, (30 watts) monopolar coagulation was performed. All excised lesions were submitted for individual biopsy confirmation. In group B, fenestration was first performed, and then the inner cyst wall was coagulated by the touch technique using 30 W current monopolar forceps. No sutures were used in either group, and the ovaries were left open. No complications recorded during or after surgery. Shifting from laparoscopy to laparotomy also not happened in any patient.
Statistical analysis method
Data were collected, revised, coded and entered into the Statistical Package for Social Science (IBM SPSS) version 22. The quantitative data were presented as mean, Standard Deviations (SDs) and ranges when their distribution found parametric and median with Inter-Quartile Range (IQR) when their distribution found non- parametric while qualitative data were presented as number and percentages. The comparison between two independent groups with qualitative data was done by using Chisquare test. The comparison between two independent groups using Independent t-test or Mann-Whitney test is appropriate. The comparison between more than two using Repeated Measures ANOVA or Friedman test is appropriate. The confidence interval was set to 95% and the margin of error accepted was set to 5%, the p-value was considered significant as the following: P>0.05: Non-significant<0.05: Significant.
Results
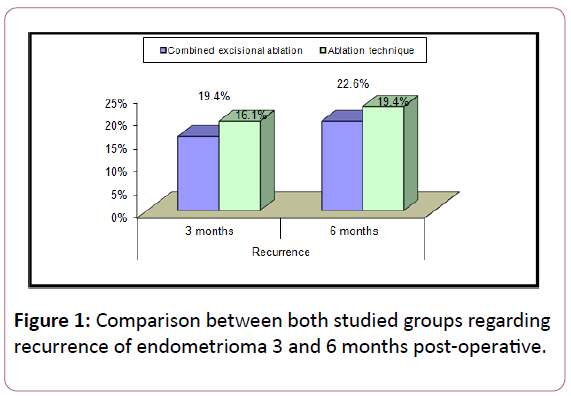
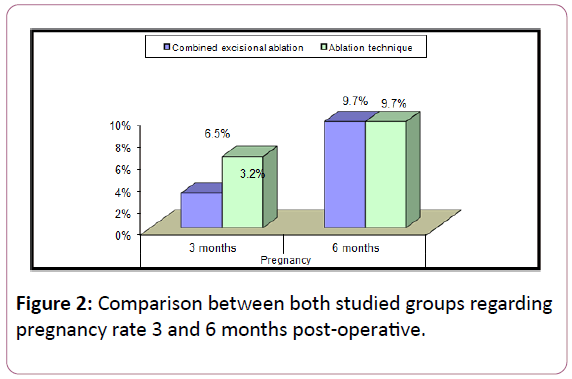
Among 62 patients, we did not record any case of failure of laparoscopy or shifting to laparotomy. The range of age in both groups was 22-36 years, demographic data and ovarian endometrioma size were comparable in both groups. The main complaint of the patient in group A was "pain and secondary infertility" while in group B, the main complaint was "Primary infertility" as shown in Tables 1 and 2. 3 patients got pregnant during the follow-up period after 3 months, 1 case in group A and 2 cases in group B and 6 patients got pregnant after 6 months of follow up, 3 cases in each group. No statistically significant difference regarding FSH level pre-operative but there was statistically significant difference after 3 months. No statistically significant difference found regarding AFC preoperative and 3 months post-operative while there was highly statistically significant difference found between both groups regarding AFC 6 months post-operative where the AFC decrease after 6 months in ablation group (Table 3). No statistically significant difference regarding volume of affected ovary preoperative and 3 months post-operative while there was statistically significant difference found 6 months post-operative where the volume decreased in patients managed by ablation after 6 months compared with the volume in group A (Table 4). There was no statistically significant difference regarding recurrence or pregnancy rates 3 and 6 months post-operative (Figures 1 and 2). Among group A, no statistically significant difference found between FSH level pre-operative and 3 and 6 months post-operative while there was statistically significant difference regarding AFC pre-operative and 3 months and 6 months post-operative. And there was statistically significant difference regarding ovarian volume pre and 3 months postoperative where there was an increase in the ovarian volume in the follow-up period (3 months) (Table 5). Among group B, statistically significant difference found between FSH level preoperative and 3 months post-operative while there was statistically significant difference in AFC pre and 6 months postoperative and in the volume of the affected ovary pre and3 months post-operative (Table 6).
| Combined excisional ablation | Ablation technique | Test value | P-value | Sig. | ||
|---|---|---|---|---|---|---|
| No.=31 | No.=31 | |||||
| Age | Mean ± SD | 28.48 ± 3.72 | 29.00 ± 3.25 | -0.582• | 0.563 | NS |
| Range | 22-36 | 22-36 | ||||
| Parity | Nullipara | 13 (41.9%) | 13 (41.9%) | 0.000* | 1 | NS |
| Multipara | 18 (58.1%) | 18 (58.1%) | ||||
| BMI | Mean ± SD | 25.63 ± 2.44 | 26.95 ± 3.16 | -1.845• | 0.07 | NS |
| Range | 21.4-31.5 | 22-34.8 | ||||
| Complain | Primary infertility | 7 (22.6%) | 13 (41.9%) | 3.159* | 0.206 | NS |
| Secondary infertility | 12 (38.7%) | 7 (22.6%) | ||||
| Pelvic pain | 12 (38.7%) | 11 (35.5%) | ||||
| Size of cyst | Mean ± SD | 5.10 ± 0.74 | 5.28 ± 0.47 | -1.124• | 0.266 | NS |
| Range | 4.2-8 | 4.5-6 |
Table 1: Comparison between the both studied groups regarding demographic data.
| Combined excisional ablation | Ablation technique | Test value• | P-value | Sig. | ||
|---|---|---|---|---|---|---|
| No.=31 | No.=31 | |||||
| FSH pre | Median (IQR) | 6 (5.3-6.6) | 5.4 (4.3-6.7) | 1.276 | 0.202 | NS |
| Range | 4-8 | 3.8-15.7 | ||||
| FSH 3 mon |
Median (IQR) | 5.85 (5.1-6.7) | 5 (4.2-6.0) | 2.855 | 0.004 | HS |
| Range | 4-8.7 | 3-14 | ||||
| FSH 6 mon | Median (IQR) | 5.4 (5-6.2) | 5.15 (4.75-6.0) | 1.44 | 0.15 | NS |
| Range | 4.3-8 | 3.7-11.9 |
Table 2: Comparison between both studied groups regarding FSH pre-operative and 3 and 6 months post-operative.
| Combined excisional ablation | Ablation technique | Test value• | P-value | Sig. | ||
|---|---|---|---|---|---|---|
| No.=31 | No.=31 | |||||
| AFC pre-operative | Median (IQR) | 3 (3-4) | 3 (3-4) | 0.668 | 0.504 | NS |
| Range | 1-7 | 2-6 | ||||
| AFC 3mon | Median (IQR) | 4 (3-4) | 4 (4-4) | 1.472 | 0.141 | NS |
| Range | 1-5 | 2-5 | ||||
| AFC 6mon | Median (IQR) | 4 (4-5) | 4 (3-4) | 2.831 | 0.005 | HS |
| Range | 1-5 | 2-4 |
Table 3: Comparison between both studied groups regarding AFC of affected ovary pre-operative and 3 and 6 months postoperative.
| Combined excisional ablation | Ablation technique | Test valueǂ | P-value | Sig. | ||
|---|---|---|---|---|---|---|
| No.=31 | No.=31 | |||||
| Volume affect | Median (IQR) | 75.3 (62.7-100.3) | 78.4 (56.4-93) | -0.021 | 0.983 | NS |
| Range | 16.5-225.9 | 32-116 | ||||
| Volume 3 mon | Median (IQR) | 10.45 (7.2-14.8) | 7.6 (4.9-10.9) | -1.805 | 0.071 | NS |
| Range | 0.4-35.2 | 2.5-41.8 | ||||
| Volume 6 mon | Median (IQR) | 11 (8-13.2) | 6.25 (4.9-10.75) | -2.954 | 0.003 | HS |
| Range | 0.51-28.3 | 1.6-37.3 |
Table 4: Comparison between both studied groups regarding the volume of affected ovary pre-operative and 3 and 6 months postoperative.
| Combined excisional ablation | Test value | P-value | Sig. | Post hoc by Wilcoxon Signed Rank test | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | 3 months | 6 months | P1 | P2 | P3 | |||||
| FSH | Median (IQR) | 6 (5.3-6.6) | 5.85 (5.1-6.7) | 5.4 (5-6.2) | 1.93 | 0.381 | NS | 0.581 | 0.226 | 0.136 |
| Range | 4-8 | 4-8.7 | 4.3-8 | |||||||
| AFC | Median (IQR) | 3 (3-4) | 4 (3-4) | 4 (4-5) | 16.78 | <0.001 | HS | 0.025 | 0.002 | 0.043 |
| Range | 1-7 | 1-5 | 1-5 | |||||||
| Volume affect | Median (IQR) | 75.3 (62.7-100.3) | 10.45 (7.2-14.8) | 11 (8-13.2) | 43.931 | 0 | HS | 0 | 0 | 0.304 |
| Range | 16.5-225.9 | 0.4-35.2 | 0.51-28.3 | |||||||
Table 5: Comparison between FSH level and AFC and volume of the affected ovary pre-operative and 3 and 6 months post-operative in (group A).
| Ablation technique | Test value | P-value | Sig. | Post hoc by Wilcoxon Signed Rank test | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | 3 months | 6 months | P1 | P2 | P3 | |||||
| FSH | Median (IQR) | 5.4 (4.3-6.7) | 5 (4.2-6.0) | 5.15 (4.75-6.0) | 6.283 | 0.043 | S | 0.01 | 0.077 | 0.63 |
| Range | 3.8-15.7 | 3-14 | 3.7-11.9 | |||||||
| AFC | Median (IQR) | 3 (3-4) | 4 (4-4) | 4 (3-4) | 11.455 | 0.003 | HS | 0.003 | 0.319 | 0.002 |
| Range | 2-6 | 2-5 | 2-4 | |||||||
| Volume affect |
Median (IQR) | 78.4 (56.4-93) | 7.6 (4.9-10.9) | 6.25 (4.9-10.75) | 43.143 | 0 | HS | 0 | 0 | 0.113 |
| Range | 32-116 | 2.5-41.8 | 1.6-37.3 | |||||||
Table 6: Comparison between FSH level and AFC and volume of the affected ovary pre-operative and 3 and 6 months post-operative in (group B).
Discussion
In this study we compared the effect of laparoscopic ablation excision and ablation alone in patients with unilateral mild to moderately sized endometrioma on AFC, ovarian volume, D2 FSH, recurrence rate of lesion and pregnancy rate defined as detection of early fetal viability.
The study found that both techniques caused diminished ovarian volume of ipsilateral ovary and FSH serum level within 6 months follow up, and increased AFC of ipsilateral ovary. But combined excision ablation group was significantly better and has less damage effect. Basal FSH concentrations decreased significantly after both intervention and more significant in excision ablation group, this was due to more developed ovarian follicles that secreting Inhibin B and Estradiol and thus affecting FSH concentrations.
We did not use Anti-Mullerian Hormone (AMH) estimation as ovarian reserve marker because of financial reason, also compared with AMH, AFC has the advantage of correlating directly with the ovarian reserve of a single ovary. But AMH being a systemic marker seems not helpful as ovarian volume and AFC in contralateral side did not change in studied groups.
The assessment of ovarian reserve remains a challenge in most of literature. Among the ultrasonographic markers of ovarian reserve, AFC is considered to be the most reliable indicator of the primordial follicle pool [5]. We have demonstrated that although AFC in ipsilateral ovary in both groups was diminished before intervention (Range=1-7) due to presence of an ovarian cyst itself causes reduced ovarian reserve in addition to difficulty or underestimation in the presence of the anatomical alteration caused by an endometrioma, but the study reported rapid increase in AFC within first visit in excision ablation than in ablation group, that because women subjected to excision had less damage to functioning ovarian tissue.
Present study demonstrated that laparoscopic surgery either ablation or excision ablation both improved pregnancy rate which considered as strongest indicator of successful treatment by surgical interventional and although it was not statistically significant but we consider any recorded pregnancy is of clinical significance. In both techniques, careful laparoscopic intervention and getting rid of diseased tissue improved pregnancy rate, improve the hormonal milieu and give a chance for growing cohort follicles to grow.
Various risk factors have been suggested for recurrence in the literature and these are both patients and surgeon related. We defined recurrence as cysts with a diameter of more than 10mm and pain recurrence, this study reported less recurrence rate in excision ablation group than ablation alone through 6 months follow up, although it was not significant but it denotes fewer residuals left after excision ablation. Recurrence of pain was totally associated with recurrence of a cyst and it was not significantly different in both groups.
In present study, laparoscopic cyst ablation by electrocoagulation alone as only treatment technique was associated with a significant decrease in ovarian volume after surgery, which is partially a consequence of the extended damage of the ovarian vascular system and it has the potential disadvantages of leaving a greater area of necrotic tissue behind, with increased inflammatory action that needs time to heal.
But in women undergone cyst excision was restricted to cyst wall which was not totally excised and haemostasis achieved with the application of a 30 W current using monopolar forceps on the cyst bed to control some bleeding points diminished its adverse effect, this technique gave a protection of ovarian cortical functioning tissue. Also, excision leaves underlying connective tissue in which rapid healing occurs.
In the present study, both techniques negatively affect ovarian volume but to a lesser extent in excision ablation group. In accordance with our study, Hesham, et al. included 100 women with bilateral mild to moderate endometriosis and compared the effect of stripping versus coagulation on ovarian reserve, they reported a reduction in ovarian volume after both techniques, especially six months after surgery, but they concluded less harmful effect to the coagulation group [5].
In agreement with the present study, Var, et al. thesis including 48 women with bilateral endometriomas randomized to either laparoscopic ovarian cystectomy or coagulation, they reported reduced ovarian volume in both groups, and the reduction in the coagulation group was more evident due to destruction of the ovarian tissue by the thermal effect [6].
The present study demonstrated an increase in AFC in both groups especially in excision group, and this reported by studies working in IVF and Intracytoplasmic Sperm Injection (ICSI) where they reported that the number of oocytes retrieved is similar in operated and non-operated ovary [7].
In accordance with our study, Muzii, et al. in their metaanalysis, concluded that ovarian reserve evaluated with AFC was not significantly impaired by surgical excision of the ovarian endometrioma when it was performed with the stripping technique [8]. They also concluded that non-excisional techniques did not affect AFC values after surgery and antral follicle of the operated ovary did not change significantly when compared with the pre-operative values of the same ovary.
Another study done in three steps by George, et al. reported that folliculogenesis based on AFC measurement was better restored, after choosing the ‘three-stage procedure’ instead of stripping for conservative laparoscopic treatment of endometriotic cysts [9]. They described three-stage procedure as primary laparoscopic drainage of endometriotic cyst followed by hormonal down-regulation for 3 months and 12 weeks later second look laparoscopy carried out to vaporize the internal wall by using a CO2 laser.
Present study recorded rapid improvement in FSH level in both groups and especially in excision group, demonstrating that the ovary produced hormones like (E2) inhibit production of FSH. In accordance, Broekmans, et al. and Jadranka, et al. reported a slight reduction in FSH level in coagulation therapy [10,11].
We did not record significant reduction of pain or recurrence in both groups, while Wright, et al. concluded good symptomatic relief at 6 months from pelvic pain for the majority of participants irrespective of the treatment modality. But the study was dealt with advanced stage of endometriosis and bilateral ovarian lesion and peritoneal spread [12].
One of the limitations faced in present study is the limited duration of follow up, also sample size was small, but postoperative observation done by the same person and we did not add any medical management to avoid masking the operation efficiency and because 2\3 of patients seeks for fertility, but regarding recurrent cases we counselled them for medical treatment options and non-pregnant cases referred to fertility clinic.
Careful patient selection, careful stripping of a cyst and diminished use of electrocoagulation will maximize outcomes like pregnancy rate and recurrence rate. The long-term effect of intervention should be evaluated on ovarian reserve and premature ovarian failure.
It seems that surgeon skills and preferences, lesion stage and patient characteristics, instruments development and refinement are responsible for this debate happening. Applying standard protocols for management could be of help, and addition of more ovarian reserve markers as AMH, Inhibin B, Doppler studies, in addition to AFC and ovarian volume will guide to perfect outcome.
Conclusion
Laparoscopic excision ablation or ablation alone for management of unilateral endometrioma ≤ 5 cm decreased ovarian volume of ipsilateral ovary and improved serum FSH level but slightly increase AFC. Ablation alone had more destructive impact on ovarian volume and AFC. Both recurrence rate and pregnancy rate were similar. Further studies with larger samples are needed to evaluate risk and benefit of different laparoscopic intervention.
Ethical approval
The protocol and all corresponding documents were declared for Ethical and Research and approval by the local ethical committee of Obstetrics and Gynaecology Department, Al-Azhar University Hospital. Informed consent was taken from each patient after explanation of the purpose and procedure of the study.
Conflict of Interest
The authors report no conflict of interest regarding the publication of this paper.
Funding
There is no source of any financial support or funding.
Acknowledgement
We thank all included women for the valuable contribution in this work.
References
- Pados G, Tsolakidis D, Assimakopoulos E, Athanatos D, Tarlatzis B (2010) Sonographic changes after laparoscopic cystectomy compared with three-stage management in patients with ovarian endometriomas: a prospective randomized study. Hum Reprod 25: 672-677.
- Hirokawa W, Iwase A, Goto M, Takikawa S, Nagatomo Y, et al. (2011) The post-operative decline in serumanti-Müllerian hormone correlates with thebilaterality and severity of endometriosis. Hum Reprod 26: 904-910.
- Benaglia L, Somigliana E, Vighi V, Ragni G, Vercellini P, et al. (2010) Rate of severe ovarian damage following surgery for endometriomas. Hum Reprod 25: 678-682.
- Noordzij M, Tripepi G, Dekker FW, Zoccali C, Tanck MW, et al. (2010) Sample size calculations: basic principles and common pitfalls. Nephrol Dial Transplant 25: 1388-1393.
- Salem HA, Hegab HM, Elkaffash DM, Azb H, Hosny TA (2013) Assessment of the ovarian reserve before and after laparoscopic surgery using two different techniques for ovarian endometrioma. IOSR-JDMS 6: 43-48.
- Var T, Batioglu S, Tonguc E, Kahyaoglu I (2011) The effect of laparoscopic ovarian cystectomy versus coagulation in bilateral endometriomas on ovarian reserve as determined by antral follicle count and ovarian volume a prospective randomized study. Fertil Steril 95: 2247-2250.
- Lima ML, Nastri CO, Coelho Neto MA, Navarro PA, Martins WP, et al. (2015) Assessment of ovarian reserve by antral follicle count in ovaries with endometrioma. Ultrasound Obstet Gynecol 46: 239-242.
- Muzii L, Di Tucci C, Di Feliciantonio M, Marchetti C, Perniola G, et al. (2014) The effect of surgery for endometrioma on ovarian reserve evaluated by antral follicle count: a systematic review and meta-analysis. Hum Reprod 29: 2190-2198.
- Visser JA, Themmen AP (2005) Anti-Müllerian hormone and folliculogenesis. Mol Cell Endocrinol 234: 81-86.
- Broekmans FJ, Kwee J, Hendriks DJ, Mol BW, Lambalk CB (2006) A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update 12: 685-718.
- Georgievska J, Sapunov S, Cekovska S, Vasilevska K (2015) Effect of Two Laparoscopic Techniques for Treatment of Ovarian Endometrioma on Ovarian Reserve. Med Arch 69: 88-90.
- Wright J, Lotfallah H, Jones K, Lovell D (2005) A randomized trial of excision versus ablation for mild endometriosis. Fertil Steril 83: 1830-1836.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences